
"Monoclonal Antibody Treatments Save Lives," announced the New York City Department of Health in an October 26 public notice. These treatments "are available and lifesaving," the agency said, noting that they "have averted at least 1,100 hospitalizations and at least 500 deaths among people treated in New York City." The agency urged the public to seek out these monoclonal antibody treatments as soon as possible: "When given early after symptom onset, mAb treatments can decrease the risk of hospitalization and death due to COVID-19, which is why it is crucial to get tested for COVID-19 as soon as symptoms begin - the sooner someone is tested, the sooner treatment can begin."
The city's health agency quoted its own Health Commissioner Dr. Dave A. Chokshi: "the science shows that monoclonal antibody treatments work and can make all the difference when it comes to the severity of COVID-19 illness." It thus urged that "treatment should be given as soon as possible after someone tests positive for COVID-19." Studies from Pfizer, cited by the agency, independently demonstrated just how effective the company's antiviral treatment, called Paxlovid, can be: it "decreased Covid-19-linked hospitalisation or mortality risk from any cause by 88%."
But with the Omicron variant now the dominant COVID strain in New York, both the city and state are facing severe shortages in the availability of effective antiviral monoclonal treatments. While Pfizer claimed its antiviral treatment would work against Omicron, the New York State Department of Health issued a memo to all health care providers this week warning that "Sotrovimab (Xevudy) is the only authorized monoclonal antibody product expected to be effective against the omicron variant." Yet due to "a significant surge in cases and reduced effectiveness of existing therapeutics due to the omicron variant," the agency warned that "supplies of oral antivirals will be extremely limited initially." As of this week, the agency also said the same of its monoclonal antibody treatment: "supplies of Sotrovimab are extremely limited."
These severe shortages mean that there will be far more people who are sick from COVID than there are available doses of antiviral and monoclonal antibodies treatment. That, in turn, requires that healthcare providers make decisions about who should be prioritized to receive such life-saving treatments and who should be deprioritized, and which factors ought to be used to determine priority.
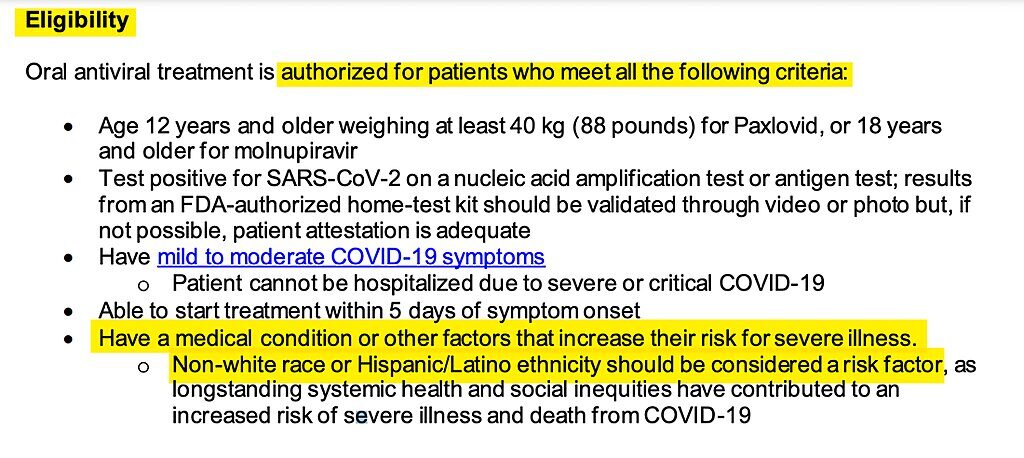
Before determining priority schemes, it must first be determined which groups of COVID patients are eligible at all to receive these potentially life-saving treatments and which from the start are declared ineligible. The state Department of Health memo sets out the list of all factors which must be met in order for a patient to be eligible. They include age (must be older than 12), COVID status (must have tested positive), and progression of the virus (must have "mild to moderate COVID-19 symptoms").
Then there is an additional requirement that makes intuitive sense: the COVID patient must "have a medical condition or other factors that increase their risk for severe illness." It makes sense that the government would seek to prioritize those who are at higher risk for developing severe illness.
But the policy then states that anyone who is non-white — regardless of age, health or underlying medical conditions — is automatically deemed to have met the requirement that one must have "a medical condition or other factors that increase their risk for severe illness" in order to receive this treatment ("Non-white race or Hispanic/Latino ethnicity should be considered a risk factor."). That means that a healthy twenty-year-old Asian football player or a 17-year-old African-American marathon runner from a wealthy family will be automatically deemed at heightened risk to develop serious COVID illness — making them instantly eligible for monoclonal treatments upon testing positive and showing symptoms — while a White person of exactly the same age and health condition from an impoverished background would not be automatically eligible.
The rationale for using race to determine who is and is not eligible for life-saving COVID treatments is dubious in the extreme, to put it generously. The last passage of the New York Health Department's memo states that "at this time, Sotrovimab (Xevudy) is the only authorized monoclonal antibody therapeutic that is expected to be effective against the omicron variant of SARS-CoV-2." It directs that "Supplies of Sotrovimab are extremely limited and providers should adhere to NYS DOH prioritization guidance."
That separate document establishes the official framework for determining not just eligibility but also prioritization in the event of limitations on the availability of COVID treatments. Entitled "Prioritization of Anti-SARS-CoV-2 Monoclonal Antibodies and Oral Antivirals for the Treatment of COVID-19 During Times of Resource Limitations," the document details the triage procedures that should be used to determine which sick people get this treatment and which patients are denied it. "In times of limited supplies of monoclonal antibodies (mAbs) and oral antivirals (OAVs), providers should prioritize patients eligible for treatment based on their level of risk for progressing to severe COVID-19," the memo states, adding: "in addition, the most efficacious products should be prioritized for patients with the highest risk for hospitalization and death."
That document sets forth five different categories of patients who are entitled to priority when it comes to limited COVID treatment. The more risk factors a patient has, the higher priority they are assigned. As one would expect, COVID patients who are older, immunocompromised, and with "risk factors for severe illness" receive priority in the event of treatment shortages. But the priority scheme also directs that race be used as a critical metric: "non-white race or Hispanic/Latino ethnicity should be considered a risk factor, as longstanding systemic health and social inequities have contributed to an increased risk of severe illness and death from COVID-19."
To justify this race-based priority scheme, the New York State memos rely on and cite two separate documents from the Centers for Disease Control (CDC). The first is entitled "People with Certain Medical Conditions," and it lists the medical conditions that render a person "more likely to get severely ill from COVID-19." On that list one finds the pathologies one would expect: cancer, diabetes, obesity, heart conditions and others. But the CDC also features race as a factor to consider when assessing risk:
Long-standing systemic health and social inequities have put various groups of people at increased risk of getting sick and dying from COVID-19, including many people from certain racial and ethnic minority groups and people with disabilities.The document which the CDC cites is exclusively devoted to elaborating on its rationale for including race as a COVID risk factor. Entitled "Risk of Severe Illness or Death from COVID-19 — Racial and Ethnic Health Disparities," it begins by asking: "Why are some racial and ethnic minority groups disproportionately affected by COVID-19?"
Studies have shown people from racial and ethnic minority groups are also dying from COVID-19 at younger ages. People in minority groups are often younger when they develop chronic medical conditions and may be more likely to have more than one condition.
The factors which the CDC cites immediately make clear how warped it is to prioritize some racial groups over others when it comes to access to life-saving COVID treatments. To begin with, the CDC notes that "people from some racial and ethnic minority groups are less likely to be vaccinated against COVID-19 than non-Hispanic White people." Indeed, the most recent CDC data demonstrates that Black people and Hispanics are getting vaccinated at lower rates than White people, while Asians are getting vaccinated at higher rates than everyone. That data shows that for forty-two states surveyed, "58% percent of White people had received at least one COVID-19 vaccine dose, which was close to the rate for Hispanic people (56%) but higher than the rate for Black people (51%)," while "the overall vaccination rate across states for Asian people was higher compared to White people (77% vs. 58%)."
But at least in many liberal sectors, a failure to be vaccinated for COVID has been deemed a moral failing that deserves deprioritization for health care, not higher prioritization. Those calling for vaccine mandates and vaccine passports want people who are unvaccinated to be denied the ability to work, study, travel or have access to public spaces on the ground that being unvaccinated is an immoral choice that endangers responsible citizens. Some doctors are refusing to provide health care to unvaccinated people, and the medical profession has been openly debating whether the unvaccinated should be turned away. Some liberal politicians have advocated that unvaccinated people be denied health insurance.
For all of 2021, the prevailing argument has been that the unvaccinated are reckless, immoral, diseased and dangerous, and deserve punishment and restrictions. But that is exactly why it was necessary to create a false narrative about who the unvaccinated population is: pretending that they are composed only of White Trump supporters while erasing the large percentages of Black and Hispanic Americans who remain unvaccinated. No liberal is comfortable admitting that they are advocating policies that will result in the firing of people in the middle of a pandemic who are disproportionately Black. Indeed, it has become increasingly popular to argue that any policy, even if racially neutral on its face, should be deemed racist if it disproportionately disadvantages Black or other non-white people; given that Black people have among the highest percentages of unvaccinated people by racial group, policies such as vaccinate mandates and passports would disproportionately result in the firing of Black workers or their denial to travel or enter other public spaces.
But whatever else is true: since when is being unvaccinated a cause for prioritizing people when it comes to life-saving COVID treatments? In liberal discourse, treating the unvaccinated as immoral monsters has become common. But unlike liberal media outlets, the CDC cannot ignore the fact that vaccination rates are lower among Black people than other racial groups. They have to grapple with that fact. And they do so by denying the universal applicability of the vaccine and claiming — with no data cited — that the reason for this high rate of vaccine hesitancy or refusal among Black Americans is racism and structural inequities rather than agency and choice.
Thus does the CDC attribute vaccination disparities among racial groups to social and economic "inequities." It is true that an inability to take off time from work may impede the ability to get vaccinated, but the Biden administration had made it a priority to ensure that vaccines are universally available in the U.S. Indeed, an extremely high percentage of adults 65 and older have received at least a first vaccine dose, demonstrating how widely available it is.
Moreover, the economic and work-related impediments to getting vaccinated are class-based factors, not race-based ones. Poverty and work conditions are more likely to impede an impoverished White person from getting vaccinated than an upper-class or upper-middle-class professional Black person. So disparities in vaccination rates cannot possibly justify prioritizing one racial group over another. If it is true that vaccination is a key metric for determining who is at risk of severe COVID illness, then vaccination status can — and should — be used to determine priority for monoclonal antibody and antiviral treatments, regardless of the race of the patient. Why should an unvaccinated Black, Hispanic or Asian patient be given priority to life-saving treatments over an unvaccinated White person?
And all of this is independent of the legal questions involved. Back in May, a federal appeals court struck down the Biden administration's racial preferences embedded in its COVID relief fund for small businesses, noting the unconstitutional irrationality and inequality of treating similarly situated citizens differently based on their race.
The key point to all of this is clear: race is irrelevant in these medical determinations. Regardless of why Black Americans are getting vaccinated at lower rates than other racial groups, the relevant risk factor is vaccination status, not race. Based on the CDC's premise that "COVID-19 vaccination reduces the risk of COVID-19 and its potentially severe complications," then a vaccinated Black person, all other factors being equal (age and health), would be at less risk for severe COVID complications than an unvaccinated White person. So it makes absolutely no sense to prioritize racial groups for treatment access based on vaccination disparities among racial groups.
The same is true for every other factor cited by the CDC to explain racial disparities in COVID outcomes. The CDC states, for instance, that "underlying medical conditions that increase risk for severe illness from COVID-19 may be more common among people from racial and ethnic minority groups." The examples the agency provides: "common underlying conditions among those who require mechanical ventilation or died included diabetes, high blood pressure, obesity, chronic kidney disease on dialysis, and congestive heart failure." It notes that "a study in New York City found that non-Hispanic Black and Hispanic or Latino people had higher obesity rates and higher COVID-19 mortality rates compared with non-Hispanic Asian and non-Hispanic White people."
But again, even if these risk factors are found more frequently in some races rather than others, it is still completely irrational to prioritize some races over others when it comes to life-saving treatments. If, as the CDC says, the key risk factors are obesity, diabetes and high blood pressure, then those health conditions should be the relevant prioritization factors regardless of the race of the individual patient who suffers from them. If the concern is the presence of these illnesses, what conceivable non-racist justification exists for prioritizing an otherwise healthy Black or Hispanic COVID patient who does not suffer from any of these health problems?
Even more importantly, what drives these disparities in health problems is not principally race but class: specifically, socioeconomic status. The CDC itself acknowledges this. The reason there is a greater rate of high blood pressure, diabetes and other illnesses in Black and Hispanic people than in White people is not because of some inherent susceptibility to those diseases due to genetics or race. It is, instead, due to socio-economic deprivation. This is how the CDC explains these health disparities:
Education, income, and wealth gaps: Inequities in access to high-quality education for people from racial and ethnic minority groups can lead to lower high school completion rates and barriers to college entrance.27 This may limit future job options and lead to lower paying or less stable jobs. People with lower paying jobs often do not have paid sick leave and cannot afford to miss work, even if they're sick, because they would not be able to pay for essential items like food or other important living needs if their income decreased. Lower income is strongly associated with morbidity and mortality. Compared with non-Hispanic White people, American Indian, non-Hispanic Black, and Hispanic or Latino people have lower household incomes and shorter life expectancies, as well as higher rates of underlying medical conditions that increase risk of severe illness from COVID-19.All of that is undoubtedly true. But these disparities, first and foremost, are about class, not race. That is why the section heading is "education, income and wealth gaps." Again, even if it is true that these economic disadvantages that heighten COVID risks are found in greater percentages among Black and Hispanics than Whites, the relevant risk factor is still class, not race. By the CDC's reasoning, an impoverished White person would face greater health care problems than a wealthy Black or Hispanic person. If socio-economic status is the determinative factor for risk of severe COVID outcomes, and one wishes to use crude racial membership to determine priority to treatments, then an Asian American and Indian-American would face the least risk of all.
Households led by Asian Americans had a median household income of $88,204 over the five year period covered by the 2015-2019 American Community Survey, the highest of any racial or ethnic group. Asian Americans make up almost 6% of the U.S. population.The only rational way — the only non-racist way — to determine priority for limited COVID treatment would be to determine access based on income or wealth, not race. But the most rational way of all would be to simply treat patients as individuals: specifically, to determine which individual patients, regardless of race, have health conditions that render them at higher risk for severe illness from COVID.
Nationwide, the median household income for 2015-2019 was $62,843. The median income for Non-Hispanic white households was $68,785. It was $51,811 for Latino-lead households and $41,935 for Black-lead households.
One could imagine a hypothetical where assigning priority to limited treatments based on race could at least be cogent if not persuasive. If a disease were inherently more dangerous to some races than others due to genetic factors, it might make sense to assign treatment priority based on race. But that has not proven to be true for COVID, nor does the CDC or the New York State Health Department even claim this is true.
Some preliminary (and disputed) studies have purported to find that South Asians have a genetic predisposition to greater risk of respiratory failure from COVID than other races (including Blacks and Hispanics). But such a finding would obviously not justify making all non-white people automatically eligible for limited COVID treatments by declaring them at higher risk for severe disease. Indeed, other equally preliminary and disputed studies have found that while non-white individuals have a higher risk of contracting COVID and being hospitalized from it, the highest mortality rates are found among White people ("racial and ethnic minority groups face a higher risk of ICU admission and COVID-19 positivity but a lower risk of mortality than White populations").
But all of these studies, besides being inconclusive, emphasize the key role played by socio-economic factors. In sum, the poorer one is, the more health problems they will have that can increase the risk of severe illness from COVID. That suggests that if public health policy is going to dispense with analyzing the actual risks of individual patients and instead decide to treat people as members of crude demographic groups, it makes far more sense for the relevant group to be based on socio-economic status rather than race.
Whatever else is true, it is genuinely extraordinary for a state agency to announce that members of certain racial groups who contract a disease and display symptoms will receive automatic eligibility for limited life-saving treatments, while members of other racial groups must demonstrate the existence of health problems before they are permitted to be similarly treated. Health policies that dictate that some races will receive preferential treatment over others when it comes to a shortage of life-saving treatments for a fatal disease should be permitted only in the rarest and most extreme cases if ever. Down that race-based road lies some extremely dark and disturbing outcomes.
Clarification, Dec. 31, 2021, 10:06 a.m. ET: This article was edited to clarify that Pfizer's Paxlovid is an antiviral treatment. The New York State Health Department's warning is that there are serious shortages of both antiviral and monoclonal antibody treatments due to the Omicron variant, and its race-based policy for eligibility and access applies to both.



[Link]