
|
| ©The New York Times Company |
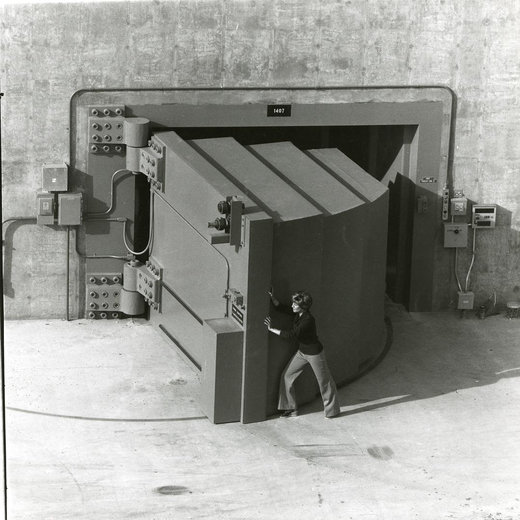
| Rosa Navarro in her apartment in Oxnard, Calif. "He died without dignity," she said of her son, Ruben. |
But what happened to Mr. Navarro quickly went from the potentially life-saving to what law enforcement officials say was criminal. In what transplant experts believe is the first such case in the country, prosecutors have charged the surgeon, Dr. Hootan C. Roozrokh, with prescribing excessive and improper doses of drugs, apparently in an attempt to hasten Mr. Navarro's death to retrieve his organs sooner.
A preliminary hearing begins here on Wednesday, with Dr. Roozrokh facing three felony counts relating to Mr. Navarro's treatment as a donor. At the heart of the case is whether Dr. Roozrokh, who studied at a transplant fellowship program at the Stanford University School of Medicine, was pursuing organs at any cost or had become entangled in a web of misunderstanding about a lesser-used harvesting technique known as "donation after cardiac death."
Dr. Roozrokh has pleaded not guilty, and his lawyer said the charges were the result of overzealous prosecutors. But the case has sent a shudder through the tight-knit field of transplant surgeons - if convicted on all counts, Dr. Roozrokh could face eight years in prison - while also worrying donation advocacy groups that organ donors could be frightened away.
"If you think a malpractice lawsuit is scaring surgeons off, wait to see what happens when people see a surgeon being charged criminally and going to jail," said Dr. Goran B. Klintmalm, president of the American Society of Transplant Surgeons, who added that he considered the case unprecedented.
David Fleming, the executive director of Donate Life America, a nonprofit group that promotes donations, said the case had "given some support to the myths and misperceptions we spend an inordinate amount of time telling people won't happen."
Mr. Fleming said about 18 people a day die in the United States waiting for transplants. That has created a tremendous demand for donor organs, and over the years the medical community has established strict protocols to govern organ harvesting.
Transplanting organs from patients whose hearts have stopped, or cardiac-death donations, began to go out of vogue in the late 1960s and early '70s after medical advances like life support and subsequent changes in the legal definition of death made donations from those declared brain dead more efficient. But health officials have encouraged cardiac-death donations in recent years.
There were 670 cardiac-death donations through the first nine months of 2007, the most in any year this decade, according to the United Network for Organ Sharing, which oversees organ allocation. Over the same period, there were 12,553 brain-dead donations, according to the network.
In brain-death donations, the donor is legally dead, but machines keep the organs viable by machines. In cardiac-death donations, after the patient's ventilator is removed, the heart slows. Once it stops, brain function ceases. Most donor protocols call for a five-minute delay before the patient is declared dead. Transplant teams are not allowed in the room of the potential donor before that.
Cardiac-death donations can make some doctors and nurses skittish if they have not previously witnessed one, said Dr. Robert Sade, the former chairman of the American Medical Association's Council on Ethical and Judicial Affairs.
"It all works exactly the same, the cuts and the procedure," Dr. Sade said. "But the circumstances are quite different."
Several days after Mr. Navarro was hospitalized at the Sierra Vista Regional Medical Center here, a decision was made to remove his ventilator. According to the criminal complaint, Dr. Roozrokh ordered excessive doses of morphine and Ativan, an anti-anxiety medicine, both of which are used to comfort dying patients. In the most shocking accusation, the complaint said Dr. Roozrokh introduced Betadine, a topical antiseptic, into Mr. Navarro's system; Betadine, the complaint said, is "a harmful substance that may cause death if ingested."
Mr. Navarro died about eight hours later of what the coroner ruled was natural causes. In the end, however, because his death was not more immediate, his organs had deteriorated too much to be usable for transplant.
Prosecutors have charged Dr. Roozrokh with felony counts of dependent adult abuse, mingling a harmful substance (Betadine) and prescribing a controlled substance (morphine and Ativan) without medical purpose.
The doctor's lawyer, M. Gerald Schwartzbach, said that Dr. Roozrokh, 34, who moved to Wisconsin from Iran when he was a toddler and excelled as a collegiate swimmer, did "nothing that adversely affected the quality or length" of Mr. Navarro's life.
"Dr. Roozrokh is a brilliant young surgeon, who has dedicated his life to saving lives," Mr. Schwartzbach said. Neither the police nor prosecutors would comment on the case.
Mr. Navarro was diagnosed with adrenoleukodystrophy, a neurological disorder, when he was 9. "He would walk like he was drunk," said his mother, Rosa, a Guatemalan immigrant. "And when he would play, he would fall like Bambi."
By his early 20s, however, Mr. Navarro's mental and physical condition had deteriorated to a point where he was placed in an assisted-care facility.
On Jan. 29, 2006, Ms. Navarro received a call from the facility that her son had been found unconscious, in cardiac and respiratory arrest, but that he had been revived and transported to Sierra Vista. His brain had been damaged from lack of oxygen.
Several days later, Ms. Navarro says she was told by a doctor at the hospital, whose name she did not know, that her son would not recover and that he would be disconnected from life support.
Ms. Navarro, a machinist from Oxnard, Calif., who is on disability, said she did not have enough money to stay another night near her son. She said that shortly after leaving the hospital, she received a call from the California Transplant Donor Network, a nonprofit organization. On a tape recording made by the network, Ms. Navarro agreed to donate her son's organs, saying she did not want him "to suffer too long."
Late on Feb. 3, a transplant team including Dr. Roozrokh arrived at the hospital.
According to a police interview with Jennifer Endsley, a nurse, the transplant team, including Dr. Roozrokh, stayed in the room during the removal of the ventilator and gave orders for medication, something that would violate donation protocol. Ms. Endsley, who stayed to watch because she had never participated in this type of procedure, also told the police that Dr. Roozrokh asked an intensive care nurse to administer more "candy" - meaning drugs - after Mr. Navarro did not die immediately after his ventilator was removed.
Mr. Schwartzbach said he would address the accusations in court. "I think a great many people, lay and medical, will realize they have been significantly misinformed," he said.
Several months after the incident, federal health officials cited the hospital for a series of lapses, including failing to grant temporary clinical privileges to Dr. Roozrokh, who was under contract with the donor network. Last February, the United Network for Organ Sharing reprimanded the California Transplant Donor Network for breaking "established protocol" in the case. The donor network declined to comment.
Ms. Navarro has filed a civil suit against Dr. Roozrokh, the donor network and other doctors in the operating room, and has settled a lawsuit against the hospital. A spokesman for the hospital, Ron Yukelson, said a plan to correct the problems had been accepted by federal health officials.
Ms. Navarro said she remained angry about the way her son's life ended.
"He didn't deserve to be like that, to go that way," she said. "He died without dignity and sympathy and without respect."
Melanie Carroll contributed reporting from San Luis Obispo, and Lawrence K. Altman from New York.


Reader Comments
to our Newsletter