Inside every single human on the planet - including you - there is a community of millions residing. It's called your microbiome, and it's made up of millions of tiny bacteria that work to help keep your body functioning. In fact, these little creatures are so abundant that they outnumber your cells by about 10 to one.
These bacteria largely live in your gut and serve a number of purposes that help your body function properly. We're getting to know the microbiome a little more, but for the most part, it is largely misunderstood.
But here's what I can tell you from what we know so far...
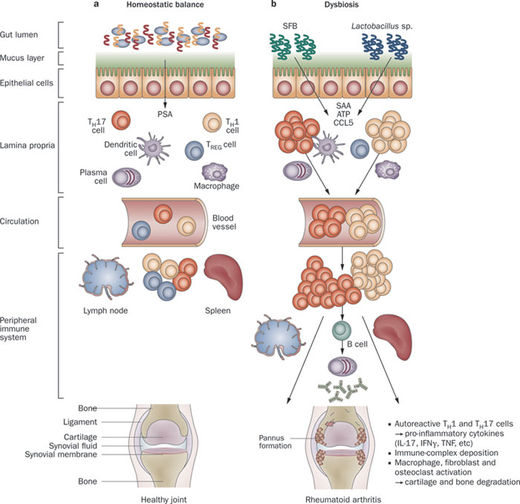
We know that these bacteria are largely good bacteria and that they live comfortably and amicably. They help to break down food, absorb nutrients, expend energy, and remove waste. They also aid in combatting foreign intruders, so you stay healthy. After all, there are even more bacteria living outside you - on every surface - that can make you sick. When one of these types of bacteria gets inside of you, your microbiome kills it. Your microbiome plays a major role in your immune system, constantly providing protection from illness of which you're likely unaware.
Your microbiome is largely determined by genetics, but it can be altered through diet and other lifestyle and environmental factors. Therefore, it is in flux depending on how you live. When you eat poorly, smoke, get older, have a hormonal imbalance, or get infected, your microbiome changes. An imbalance is created, and this can cause a number of problems.
One of which may be rheumatoid arthritis.
I recently read about this research team who did some tests on patients to take a look at their microbiomes. They examined fecal matter from patients who fell into the following three groups: those who were healthy; those who had chronic, treated rheumatoid arthritis; or those who had just been diagnosed with rheumatoid arthritis.
What they found was that patients with newly diagnosed rheumatoid arthritis had a substantially higher number of a bacteria strain called Prevotella copri (P. copri) compared to the healthy individuals and patients with chronic, treated rheumatoid arthritis. Furthermore, growth of P. copri was associated with lower amounts of beneficial gut bacteria.
This is interesting because gut bacteria has been previously linked to autoimmune disorders and inflammation. And although rheumatoid arthritis is genetic, it can also be affected by lifestyle and environmental factors, like the ones I listed earlier. So basically, the only common denominator for causation of rheumatoid arthritis is an imbalanced microbiome.
Now, it's very important to mention that this is still in the early stages of exploration and a lot more work has to be done. For starters, researchers need to learn whether or not elevated P. copri is a cause or consequence of rheumatoid arthritis. Once they learn that, they have to learn how to treat it. It is conceivable, however, that a probiotic supplement might help.
Currently, the known way to improve or encourage a healthy, balanced microbiome is through dietary measures. A healthy, balanced diet is reflected in your microbiome, and eating foods with probiotics and prebiotics is a great way to keep flora energized and effective - and maybe even prevent the onset of arthritis.
Sources for Today's Article:
- Deardorff, J., "Gut Bacteria Linked to Rheumatoid Arthritis," Chicago Tribune web site, July 2, 2014; .
- Bornigen, D., "Functional Profiling of the Gut-Microbiome in Disease-Associated Inflammation," National Institutes of Health web site, July 31, 2013; .


Comment: Proper diet is important to the functioning of the immune system. Research has shown that gluten consumption is connected with a number of auto-immune diseases, among them rheumatoid arthritis. See:
Gluten Sensitivity and Rheumatoid Arthritis - Is There A Connection?
Lectins, Gluten, Rheumatoid Arthritis, & Molecular Mimicry