The World Health Organization considers antibiotic resistance one of the biggest threats of the 21st century. The World Economic Forum calls it a "potential disaster" for human health and the global economy. Just one such microbial threat, multidrug-resistant Staphylococcus aureus, caused more than 11,000 deaths in the United States in 2011 alone, and that one plus other resistant microbes kill hundreds of thousands of people annually around the world.
How has this happened? By a combination of Darwinian natural selection (hit a population of bacteria with an antibiotic, and the fittest will survive) and an evolutionary mechanism discovered much more recently, a phenomenon so counterintuitive that Charles Darwin didn't imagine it: horizontal gene transfer. What that means is genes moving sideways across boundaries-between individuals, between species, even between kingdoms of creatures. One researcher in the 1950s dubbed it "infective heredity." Genome sequencing reveals that such horizontal transfer of DNA has been profoundly important in the history of life, and among bacteria it's especially common, with particular implications for the spread of antibiotic-resistance genes.
Comment: Darwin's theory of evolution is very much up for question: Orphan genes, and the problem they pose for evolution
At the start of the 1960s, a Japanese scientist named Tsutomu Watanabe saw this coming. After years of collaboration with Japanese colleagues, in 1963 he published a paper in English and, adopting the earlier phrase, called the phenomenon of antibiotic resistance "an example of 'infective heredity.'"
The Japanese work began after World War II in response to increased cases of bacillary dysentery. Postwar deprivation, dislocation, and disruption of sanitary and health services probably exacerbated the problem, but its proximate cause was infection by bacteria of the Shigella genus. The preferred treatment first was sulfa drugs; when Shigella strains showed resistance to them, medical people turned to newer antibiotics, such as streptomycin and tetracycline.
By 1953 strains of Shigella showed resistance to both of those also. Each bacterial strain, though, was resistant to only one drug. It could still be stopped by the others. Then in 1955 a Japanese woman returned from a stay in Hong Kong sick with dysentery, and Shigella from her feces tested resistant to multiple antibiotics. From that point, resistance spread fast, and during the late 1950s Japan suffered a wave of dysentery outbreaks caused by Shigella superbugs resistant to four kinds of antibiotics: sulfas, streptomycin, tetracycline, and chloramphenicol.
The alarm bell rang louder when researchers discovered that this phenomenon wasn't confined to Shigella. Some cultures of Escherichia coli, taken from patients with resistant Shigella, showed resistance to the same drugs. So it seemed E. coli had shared. A whole packet of resistance genes had evidently moved sideways, probably in the depths of patients' guts, from one kind of bacterium to another. And the exchange wasn't limited to Shigella and E. coli. Further research showed that the packet could cross boundaries between other species, even from genus to genus, among almost every group of enteric bacteria, a large family of bugs that live within human intestines.
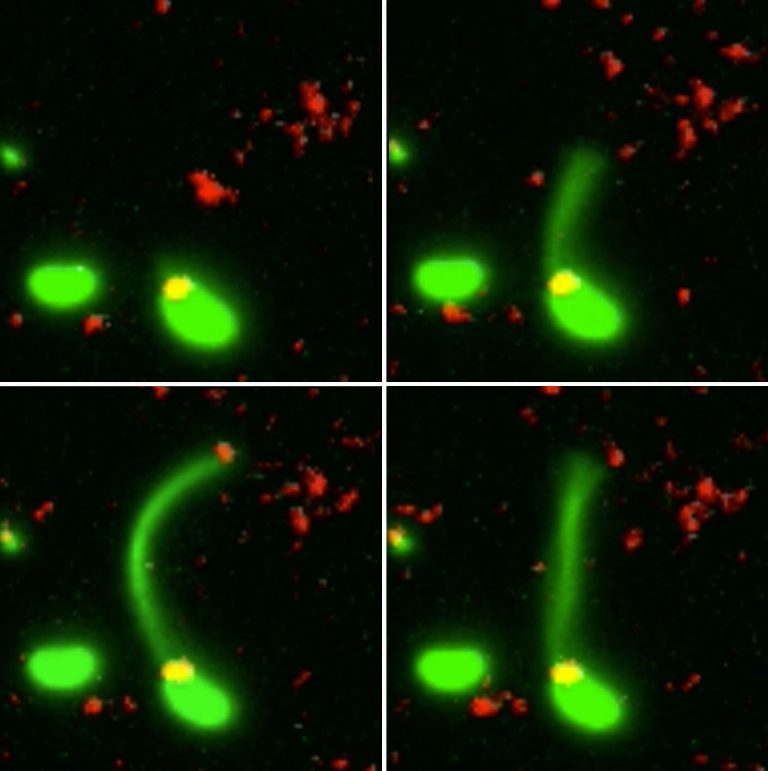
What exactly was this packet of genes that traveled so easily across boundaries? Watanabe and a colleague, Toshio Fukasawa, offered a hypothesis: It was an episome, a sort of autonomous genetic element that floats free within a bacterial cell, unattached to the cell's single chromosome. An episome is a short stretch of DNA, sometimes circular like a small bracelet, that exists and replicates in a cell independently of the cell's chromosome. It codes for traits that might be unnecessary for normal life but useful in emergencies, such as drought tolerance or immunity to a poison.
Watanabe declared to the scientific world, in his 1963 paper, what Fukasawa and he had already said in Japanese: Multiple resistance, to streptomycin and those three other antibiotics, was coded on an episome. That episome explained how harmless bacteria such as ordinary E. coli could convey genes for multiple antibiotic resistance across species boundaries, into dangerous bacteria such as Shigella dysenteriae, in a blink. The word "episome" would later be replaced by a synonym, "plasmid." Scientists now recognize plasmids as a major mechanism for transferal of antibiotic-resistance genes - sometimes whole packets of genes for multiple resistance - from one species of bacterium to another.
Among the most sobering recent developments was the announcement by a Chinese team of scientists two years ago that they had found a gene for resistance to colistin - a last-ditch antibiotic that has been called "critically important for human medicine" - in a strain of E. coli isolated from a pig. They named the gene mcr-1. What made their discovery especially chilling was that mcr-1 rode on a plasmid, meaning that it could pass easily, quickly, from one species of bacterium to another by horizontal transfer.
Soon after the Chinese announcement came a flurry of publications from other groups of scientists declaring that they too had found the mcr-1 gene on bacterial plasmids - in the urine of an 83-year-old Swiss man, in Danish chicken meat, in piglets from Flanders, in the feces of a hospitalized child in Cambodia, and elsewhere. This means that colistin too may soon be ineffective against many kinds of multidrug-resistant bacteria.
In the meantime, the influence of Tsutomu Watanabe had reached far. A young American named Stuart B. Levy, on leave from medical school for a research fellowship, heard about him and arranged to work for a few months of 1962 in Watanabe's lab, at Keio University in Tokyo. It was a formative experience.
Stuart Levy, M.D., is nowadays a professor at Tufts University School of Medicine and an internationally renowned authority on antibiotic use, overuse, and resistance. He reminisced about Watanabe when I visited him in his office, on the eighth floor of a drab building just outside Boston's Chinatown.
"We worked in the lab without air-conditioning," Levy said. "It was very, very hot. Hot and humid." Levy's lab bench was on an upper level, with a sort of overlook from which, glancing down, he could see Professor Watanabe doing experiments in short sleeves "because it was so hot." Periodically someone would bring forth a hose and spray the professor with water to cool him off. A small man, an inch or two shorter than Levy, Watanabe spoke impeccable English and had a straightforward manner toward students and postdocs. He would bicycle around campus with his junior colleagues and sometimes take a few out to a bar for an evening of karaoke. On a visit to Philadelphia for a scientific meeting, Watanabe stayed with Levy's parents, who lived nearby. "I was delighted," Levy said, "because I worshipped him, in a weird way." A lively mentor, a focused and dignified Japanese scientist. What became of Watanabe? I wondered.
"He passed away of stomach cancer," said Levy. "He probably was in his 40s, early 50s."
After finishing his medical studies, Levy pursued a lifelong mission of trying to protect the world against bacterial superbugs. In 1992 he published a book titled The Antibiotic Paradox - the paradox being that these drugs, which made human lives so much better and longer during the 20th century, have also been making our bacterial enemies far more formidable by forcing them to adapt to the evolutionary challenge. Levy wrote that the spread of plasmid-transferable resistance genes, back in Watanabe's time, had "opened the eyes of microbiologists and medical scientists to a breadth of gene spread never before imagined."
The implications weren't broadly comprehended then-but nowadays they are, sweeping around the planet as fast as a gene can jump sideways.
This story appears in the September 2018 issue of National Geographic magazine.


Comment: For more on the profound implications of horizontal gene transfer, see:
- Lethal Sex -The Rise of Sexually Transmitted Diseases in the Age of Postmodernist Liberalism
- Jumping genes: Cross species transfer has driven evolution
- Scientists observe bacteria 'harpooning' DNA
- Brain-eating amoeba found in Louisiana water system - Again
- Darwin, we've got a problem: Reverse speciation and environmentalists playing god
Also check out SOTT radio's:- The Truth Perspective: Are Cells the Intelligent Designers? Why Creationists and Darwinists Are Both Wrong
- The Health & Wellness Show: Syphilitic Superpower: The rise of STDs
And for a fascinating visualization of DNA at work, check out the following video: