
A microRNA called miR-30c-5p contributes to nerve pain in rats and people, a new study finds. A different microRNA, miR-711, interacts with a well-known itch-inducing protein to cause itching, a second study concludes. Together, the research highlights the important role that the small pieces of genetic material can play in nerve cell function, and may help researchers understand the causes of chronic nerve pain and itch.
MicroRNAs help regulate gene activity and protein production. The small molecules play a big role in controlling cancer (SN: 8/28/10, p. 18) and other aspects of health and disease (SN: 2/20/16, p. 18). Usually, microRNAs work by pairing up with bigger pieces of RNA called messenger RNAs, or mRNA. Messenger RNAs contain copies of genetic instructions that are read by cellular machinery to build proteins. When microRNAs glom onto the messengers, the mRNA can be degraded or the microRNAs can prevent the protein-building machinery from reading the instructions. Either way, the result is typically to dial down production of certain proteins.
In the case of nerve pain, miR-30c-5p limits production of an important protein called TGF-beta that's involved in controlling pain, María Hurlé, a pharmacologist at the University of Cantabria in Santander, Spain, and colleagues report August 8 in Science Translational Medicine. The researchers discovered the link in experiments with mice, rats and people.
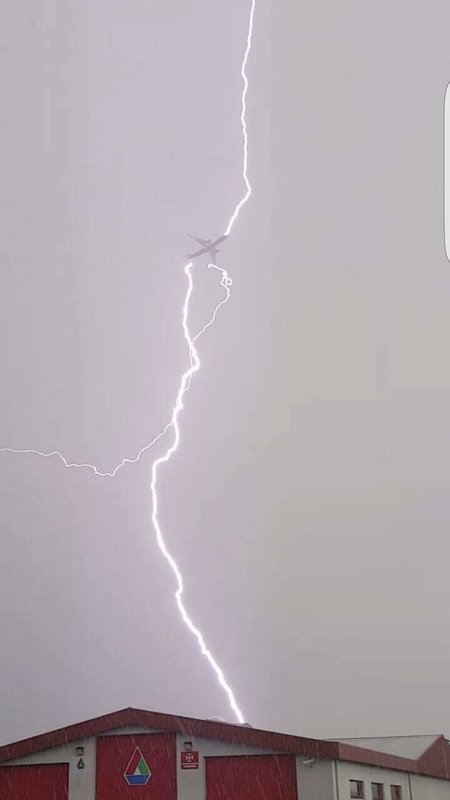
In the rat experiments, researchers cut the sciatic nerve in the thigh, making the rodents more sensitive to pain caused by heat or cold. These rats had more miR-30c-5p in their blood and cerebral spinal fluid than uninjured rats did, Hurlé and colleagues found. And the amount of the microRNA in the rats' blood correlated with their pain sensitivity. People with nerve pain caused by a lack of blood flow to a limb also had elevated levels of the microRNA in their blood and spinal fluid.
But the finding doesn't mean that doctors can treat nerve pain by blocking the microRNA in people, she says. Both the microRNA and TGF-beta do too many other important jobs throughout the body to mess with them. The research, however, does suggest that the level of miR-30c-5p in people's blood and spinal fluid might be a good indicator of nerve pain.
Having a nerve pain indicator would be useful, says Marzia Malcangio, a neuropharmacologist at King's College London who was not involved in either study. Pain doctors don't know of any biological molecules that can distinguish nerve pain from pain caused by inflammation or other causes, Malcangio says. Making that distinction is important because different types of pain are treated differently.
A different microRNA, miR-711, seems to be the culprit causing chronic itching in people with lymphoma, neurobiologist and pain researcher Ru-Rong Ji and colleagues report in the Aug. 8 Neuron.
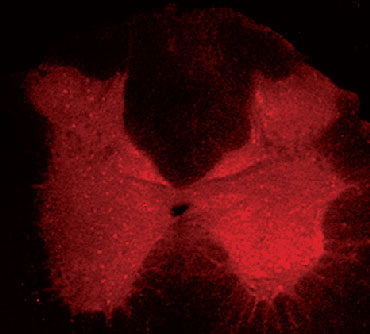
Cancerous immune cells called T-cells secrete miR-711, the team showed in experiments with mice. And giving mice the microRNA by itself made the rodents scratch. Surprisingly, the researchers found, the microRNA gloms onto a well-known pain and itch sensing protein called TRPA1 outside of a cell, instead of binding to an mRNA inside a cell like other microRNAs.
That finding may be a big advance in understanding how itch works, Malcangio says. Chemicals that trigger TRPA1 from inside a nerve cell open a floodgate that allows calcium to pour in and launch a pain signal. Tickling TRPA1 with the microRNA on the outside of the cell causes just a trickle of calcium into the nerve, producing itch instead of pain, Ji, of Duke University School of Medicine, and colleagues propose.
The team designed a peptide (a small protein or portion of a protein) that could block miR-711 from binding to TRPA1. Itchy mice that got the blocking peptide scratched about half as often as mice that got miR-711 injections alone.
Ji thinks the blocking peptide may be able to reduce itch in lymphoma patients, but the team needs to do more research before giving it to people. About a third of Hodgkin's lymphoma patients and 15 percent of people with non-Hodgkin's lymphoma have severe itching. The researchers are also investigating whether the microRNA is involved in other types of itchy conditions, such as eczema.


Comment: More on RNA: