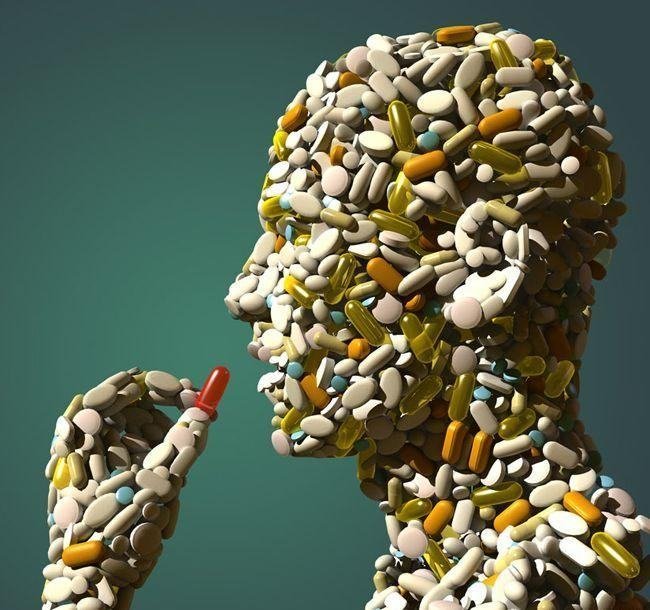
In a series of papers and comments published in The Lancet, Vikas Saini, and his colleagues provide a framework for thinking about how to address the inequities in the provision of affordable healthcare to people. The analysis addresses inequity in both high-income countries (HICs) as well as low and middle-income countries (LMICs). Their hope is to spark "serious discussions about what kind of health system we want for the 21st century as part of our commitment to universal health coverage." They believe that overuse (the provision of medical services that are more likely to cause harm than good and underuse (the failure to use effective and affordable medical interventions) of medical services takes away from "right care."
"In its simplest definition it (right care) is care that weighs up benefits and harms, is patient-centred (taking individual circumstances, values, and wishes into account), and is informed by evidence, including cost-effectiveness."In the paper that focuses on evidence for overuse of medical services, the authors Brownlee and her colleagues make a distinction between services that are clearly and universally beneficial when used on the right patient and services that are definitely inappropriate. However, they point out, most services lie within a "grey zone" where the risk-benefit profile varies widely depending on the patient (e.g. antidepressants for adolescents). Moreover, decision making in providing these services is often based on physician assumptions and biases rather than being grounded in client preferences. They report on overuse measured in two ways - directly through registries and medical records and indirectly, through geographical variation in service utilization that is not linked to the populations serviced.
Overdiagnosis
The authors link overuse of services to overdiagnosis. This refers to the process by which an illness label is assigned to a condition that will not progress if left untreated. It can occur as a result of screening tests, including those that are recommended screening procedures. Overdiagnosis is also linked to the narrowing the definition of health or, in other words broadening the definition of disease - also referred to as overmedicalization - for which the risk-benefit profile of treatment favors risk. An example of this is the lowering of thresholds to treat cholesterol.
Some of the findings highlighted in this paper are
- Antibiotics are the medication that are most appropriately overused in HICs and LMICs - for example in the Italy, 9% of children with acute diarrhea receive antibiotics inappropriately whereas in China 57% of patients do.
- There is a high rate of screening that is probably unrequired for cervical cancer, use of mammography and colonoscopy screening. In Korea, 99.7 - 99.9% of screen-detected thyroid cancers represent overdiagnosis, whereas in India there is evidence of inappropriate breast cancer screening.
- There is a lack of systematic analyses of inappropriate use of diagnostic tests but the ones of note that have been studied as overused are colonoscopy and endoscopy.
- Surgery is likely overused in HICs. Several cardiovascular procedures are overused worldwide.
- The rates of inappropriate hospital admission across the would ranges from 1% to 54%, which may represent an underuse of less aggressive treatments.
- Aggressive care is overused for end-of-life care, whereas palliative treatment is underused. About half of the people worldwide die in a hospital as a result even though a majority would prefer to die at home.
In conclusion, the authors note that even though evidence for overuse exists, there still exists the challenge of measuring it and studying it systematically.
****
Brownlee, S., Chalkidou, K., Doust, J., Elshaug, A. G., Glasziou, P., Heath, I., . . . Korenstein, D. Evidence for overuse of medical services around the world. The Lancet. doi:10.1016/S0140-6736(16)32585-5 (Abstract)



hello there,
if you are HIV positive and you want to eradicate the disease completely like i did, then don't waste time and contact doctor: dako.herbalist@gmail.com
A friend recommended him to me that his treatment is very effective, i was skeptical but i gave it a try and it worked! i went to four different hospitals to test my status they all came back negative.
and he also cure other deadly disease like Coronary Artery Disease (Ischemic Heart Disease),stroke,Chronic Obstructive Pulmonary Disease (COPD)Lower Respiratory Infection, Trachea, Bronchus, and Lung Cancers, Diarrhea Diseases etc
i can't keep this info to myself that is why i am recommending him to all that are positive or have other infections to subscribe to his treatment. Save a life and share this message with friends and family
You will surely thank me later.