|
| ©New Yorker |
| Disabled retroviruses-fossils of molecular battles that raged for generations-make up eight per cent of the human genome. |
Thierry Heidmann's office, adjacent to the laboratory he runs at the Institut Gustave Roussy, on the southern edge of Paris, could pass for a museum of genetic catastrophe. Files devoted to the world's most horrifying infectious diseases fill the cabinets and line the shelves. There are thick folders for smallpox, Ebola virus, and various forms of influenza. SARS is accounted for, as are more obscure pathogens, such as feline leukemia virus, Mason-Pfizer monkey virus, and simian foamy virus, which is endemic in African apes. H.I.V., the best-known and most insidious of the viruses at work today, has its own shelf of files. The lab's beakers, vials, and refrigerators, secured behind locked doors with double-paned windows, all teem with viruses. Heidmann, a meaty, middle-aged man with wild eyebrows and a beard heavily flecked with gray, has devoted his career to learning what viruses might tell us about AIDS and various forms of cancer. "This knowledge will help us treat terrible diseases," he told me, nodding briefly toward his lab. "Viruses can provide answers to questions we have never even asked."
Viruses reproduce rapidly and often with violent results, yet they are so rudimentary that many scientists don't even consider them to be alive. A virus is nothing more than a few strands of genetic material wrapped in a package of protein - a parasite, unable to function on its own. In order to survive, it must find a cell to infect. Only then can any virus make use of its single talent, which is to take control of a host's cellular machinery and use it to churn out thousands of copies of itself. These viruses then move from one cell to the next, transforming each new host into a factory that makes even more virus. In this way, one infected cell soon becomes billions.
Nothing - not even the Plague - has posed a more persistent threat to humanity than viral diseases: yellow fever, measles, and smallpox have been causing epidemics for thousands of years. At the end of the First World War, fifty million people died of the Spanish flu; smallpox may have killed half a billion during the twentieth century alone. Those viruses were highly infectious, yet their impact was limited by their ferocity: a virus may destroy an entire culture, but if we die it dies, too. As a result, not even smallpox possessed the evolutionary power to influence humans as a species - to alter our genetic structure. That would require an organism to insinuate itself into the critical cells we need in order to reproduce: our germ cells. Only retroviruses, which reverse the usual flow of genetic code from DNA to RNA, are capable of that. A retrovirus stores its genetic information in a single-stranded molecule of RNA, instead of the more common double-stranded DNA. When it infects a cell, the virus deploys a special enzyme, called reverse transcriptase, that enables it to copy itself and then paste its own genes into the new cell's DNA. It then becomes part of that cell forever; when the cell divides, the virus goes with it. Scientists have long suspected that if a retrovirus happens to infect a human sperm cell or egg, which is rare, and if that embryo survives - which is rarer still - the retrovirus could take its place in the blueprint of our species, passed from mother to child, and from one generation to the next, much like a gene for eye color or asthma.
When the sequence of the human genome was fully mapped, in 2003, researchers also discovered something they had not anticipated: our bodies are littered with the shards of such retroviruses, fragments of the chemical code from which all genetic material is made. It takes less than two per cent of our genome to create all the proteins necessary for us to live. Eight per cent, however, is composed of broken and disabled retroviruses, which, millions of years ago, managed to embed themselves in the DNA of our ancestors. They are called endogenous retroviruses, because once they infect the DNA of a species they become part of that species. One by one, though, after molecular battles that raged for thousands of generations, they have been defeated by evolution. Like dinosaur bones, these viral fragments are fossils. Instead of having been buried in sand, they reside within each of us, carrying a record that goes back millions of years. Because they no longer seem to serve a purpose or cause harm, these remnants have often been referred to as "junk DNA." Many still manage to generate proteins, but scientists have never found one that functions properly in humans or that could make us sick.
Then, last year, Thierry Heidmann brought one back to life. Combining the tools of genomics, virology, and evolutionary biology, he and his colleagues took a virus that had been extinct for hundreds of thousands of years, figured out how the broken parts were originally aligned, and then pieced them together. After resurrecting the virus, the team placed it in human cells and found that their creation did indeed insert itself into the DNA of those cells. They also mixed the virus with cells taken from hamsters and cats. It quickly infected them all, offering the first evidence that the broken parts could once again be made infectious. The experiment could provide vital clues about how viruses like H.I.V. work. Inevitably, though, it also conjures images of Frankenstein's monster and Jurassic Park.
"If you think about this for five minutes, it is wild stuff," John Coffin told me when I visited him in his laboratory at Tufts University, where he is the American Cancer Society Research Professor. Coffin is one of the country's most distinguished molecular biologists, and was one of the first to explore the role of endogenous retroviruses in human evolution. "I understand that the idea of bringing something dead back to life is fundamentally frightening," he went on. "It's a power that science has come to possess and it makes us queasy, and it should. But there are many viruses that are more dangerous than these - more infectious, far riskier to work with, and less potentially useful.''
Thanks to steady advances in computing power and DNA technology, a talented undergraduate with a decent laptop and access to any university biology lab can assemble a virus with ease. Five years ago, as if to prove that point, researchers from the State University of New York at Stony Brook "built" a polio virus, using widely available information and DNA they bought through the mail. To test their "polio recipe," they injected the virus into mice. The animals first became paralyzed and then died. ("The reason we did it was to prove that it can be done,'' Eckard Wimmer, who led the team, said at the time. "Progress in biomedical research has its benefits and it has its downside.'') The effort was widely seen as pointless and the justification absurd. "Proof of principle for bioterrorism,'' Coffin called it. "Nothing more." Then, two years ago, after researchers had sequenced the genetic code of the 1918 flu virus, federal scientists reconstructed it, too. In that case, there was a well-understood and highly desired goal: to develop a vaccine that might offer protection against future pandemics.
Resurrecting an extinct virus is another matter. Still, if Heidmann had stuck to scientific nomenclature when he published his results, last fall, few outside his profession would have noticed. A paper entitled "Identification of an Infectious Progenitor for the Multiple-Copy HERV-K Human Endogenous Retroelements,'' which appeared in the journal Genome Research, was unlikely to cause a stir. Heidmann is on a bit of a mission, though. He named the virus Phoenix, after the mythical bird that rises from the ashes, because he is convinced that this virus and others like it have much to tell about the origins and the evolution of humanity.
With equal ardor but less fanfare, scientists throughout the world have embarked on similar or related projects. One team, at the Aaron Diamond AIDS Research Center, in New York, recently created an almost identical virus. In the past few months, groups at Oxford University and at the Fred Hutchinson Cancer Research Center, in Seattle, have also produced results that provide startling observations about evolution and disease. The approaches often differ, but not the goals. All of these researchers hope that excavating the molecular past will help address the medical complexities that we confront today. Almost incidentally, they have created a new discipline, paleovirology, which seeks to better understand the impact of modern diseases by studying the genetic history of ancient viruses.
"This is something not to fear but to celebrate,'' Heidmann told me one day as we sat in his office at the institute, which is dedicated to the treatment and eradication of cancer. Through the window, the Eiffel Tower hovered silently over the distant city. "What is remarkable here, and unique, is the fact that endogenous retroviruses are two things at once: genes and viruses. And those viruses helped make us who we are today just as surely as other genes did. I am not certain that we would have survived as a species without them."
He continued, "The Phoenix virus sheds light on how H.I.V. operates, but, more than that, on how we operate, and how we evolved. Many people study other aspects of human evolution - how we came to walk, or the meaning of domesticated animals. But I would argue that equally important is the role of pathogens in shaping the way we are today. Look, for instance, at the process of pregnancy and birth.'' Heidmann and others have suggested that without endogenous retroviruses mammals might never have developed a placenta, which protects the fetus and gives it time to mature. That led to live birth, one of the hallmarks of our evolutionary success over birds, reptiles, and fish. Eggs cannot eliminate waste or draw the maternal nutrients required to develop the large brains that have made mammals so versatile. "These viruses made those changes possible,'' Heidmann told me. "It is quite possible that, without them, human beings would still be laying eggs."
H·I.V., the only retrovirus that most people have heard of, has caused more than twenty-five million deaths and infected at least twice that number of people since the middle of the twentieth century, when it moved from monkey to man. It may be hard to understand how organisms from that same family, and constructed with the same genes, could have played a beneficial, and possibly even essential, role in the health and development of any species. In 1968, Robin Weiss, who is now a professor of viral oncology at University College London, found endogenous retroviruses in the embryos of healthy chickens. When he suggested that they were not only benign but might actually perform a critical function in placental development, molecular biologists laughed. "When I first submitted my results on a novel 'endogenous' envelope, suggesting the existence of an integrated retrovirus in normal embryo cells, the manuscript was roundly rejected,'' Weiss wrote last year in the journal Retrovirology. "One reviewer pronounced that my interpretation was impossible.'' Weiss, who is responsible for much of the basic knowledge about how the AIDS virus interacts with the human immune system, was not deterred. He was eager to learn whether the chicken retroviruses he had seen were recently acquired infections or inheritances that had been passed down through the centuries. He moved to the Pahang jungle of Malaysia and began living with a group of Orang Asli tribesmen. Red jungle fowl, an ancestor species of chickens, were plentiful there, and the tribe was skilled at trapping them. After collecting and testing both eggs and blood samples, Weiss was able to identify versions of the same viruses. Similar tests were soon carried out on other animals. The discovery helped mark the beginning of a new approach to biology. "If Charles Darwin reappeared today, he might be surprised to learn that humans are descended from viruses as well as from apes," Weiss wrote.
Darwin's surprise almost certainly would be mixed with delight: when he suggested, in "The Descent of Man" (1871), that humans and apes shared a common ancestor, it was a revolutionary idea, and it remains one today. Yet nothing provides more convincing evidence for the "theory" of evolution than the viruses contained within our DNA. Until recently, the earliest available information about the history and the course of human diseases, like smallpox and typhus, came from mummies no more than four thousand years old. Evolution cannot be measured in a time span that short. Endogenous retroviruses provide a trail of molecular bread crumbs leading millions of years into the past.
Darwin's theory makes sense, though, only if humans share most of those viral fragments with relatives like chimpanzees and monkeys. And we do, in thousands of places throughout our genome. If that were a coincidence, humans and chimpanzees would have had to endure an incalculable number of identical viral infections in the course of millions of years, and then, somehow, those infections would have had to end up in exactly the same place within each genome. The rungs of the ladder of human DNA consist of three billion pairs of nucleotides spread across forty-six chromosomes. The sequences of those nucleotides determine how each person differs from another, and from all other living things. The only way that humans, in thousands of seemingly random locations, could possess the exact retroviral DNA found in another species is by inheriting it from a common ancestor.
Molecular biology has made precise knowledge about the nature of that inheritance possible. With extensive databases of genetic sequences, reconstructing ancestral genomes has become common, and retroviruses have been found in the genome of every vertebrate species that has been studied. Anthropologists and biologists have used them to investigate not only the lineage of primates but the relationships among animals - dogs, jackals, wolves, and foxes, for example - and also to test whether similar organisms may in fact be unrelated.
Although it is no longer a daunting technical task to find such viruses, or their genes, figuring out the selective evolutionary pressures that shaped them remains difficult. Partly, that is because the viruses mutate with such speed. H.I.V. can evolve a million times as fast as the human-immune-system cells it infects. (Such constant change makes it hard to develop antiviral drugs that will remain effective for long, and it has also presented a significant obstacle to the development of an AIDS vaccine.)
There are retroviruses (like H.I.V.) that do not infect sperm or egg cells. Because they are not inherited, they leave no trace of their history. "We can have a fossil record only of the viruses that made it into the germ line,'' Paul Bieniasz told me. "And, of course, most did not." Bieniasz is a professor of retrovirology at the Aaron Diamond AIDS Research Center and the chief of the retrovirology laboratory at Rockefeller University. He has long been interested in the way complex organisms interact with viruses and adapt to them. "With flu virus, you can watch it change in real time,'' he said. "You can watch the antibodies develop and see when and how it dies out. But with these others you are looking back tens of millions of years, so it is hard to know how a virus functioned.''
While Heidmann was working with the Phoenix virus in France, Bieniasz and two colleagues at Aaron Diamond initiated a similar project. (At first, neither team was aware of the other's work.) Bieniasz rebuilt the youngest extinct retrovirus in the human genome - one that was still active a few hundred thousand years ago - because it had the fewest mutations. The team took ten versions of that virus (we carry more than thirty) and compared the thousands of nucleotides in the genetic sequence of each version. They were almost identical, but where they differed the researchers selected the nucleotides that appeared most frequently. That permitted them to piece together a working replica of the extinct retrovirus. "If you have a person with a lethal defect in the heart,'' Bieniasz explained, "and another with a lethal defect in the kidney, you could make one healthy person by transplanting the respective organs. That is what we did.
"In the past, you got sick and you keeled over and died,'' he said. "Or you survived. Nobody could make much sense of it. But almost ten per cent of our DNA consists of old retroviruses, and that says to me that it's pretty clear they played a major role in our evolution. We evolved remarkably sophisticated defenses against them, and we would have done that only if their impact on human populations had been quite severe. It's very likely that we have been under threat from retroviruses many times throughout human history. It is eminently possible that this is not the first time we have been colonized by a virus very much like H.I.V."
At the end of the nineteenth century, a mysterious series of cancer epidemics devastated American poultry farms. One bird would fall ill and the entire flock would soon be dead. In 1909, a desperate farmer from Long Island brought a chicken with a tumor to the laboratory of Peyton Rous, a young cancer researcher at the Rockefeller Institute for Medical Research, in New York City (which became Rockefeller University). Cancer was not supposed to spread by virus, but the bird clearly had cancer. Rous, who as a young man worked on a Texas cattle ranch, was mystified. He extracted cancer cells from the sick bird, chopped them up, and injected the filtered remains into healthy chickens: they all developed tumors. A virus had to be the cause, but for years no one could figure out how the virus functioned.
Then, in the nineteen-sixties, Howard Temin, a virologist at the University of Wisconsin, began to question the "central dogma" of molecular biology, which stated that genetic instructions moved in a single direction, from the basic blueprints contained within our DNA to RNA, which translates those blueprints and uses them to build proteins. He suggested that the process could essentially run in the other direction: an RNA tumor virus could give rise to a DNA copy, which would then insert itself into the genetic material of a cell. Temin's theory was dismissed, like most fundamental departures from conventional wisdom. But he never wavered. Finally, in 1970, he and David Baltimore, who was working in a separate lab, at the Massachusetts Institute of Technology, simultaneously discovered reverse transcriptase, the special enzyme that can do exactly what Temin predicted: make DNA from RNA.
The discovery has had a profound impact on modern medicine. It not only explained how cancer can be caused by a virus but provided researchers with the tools they needed to understand the origins and natural progression of diseases like AIDS. It also created a new field, retrovirology, and, more than that, as the Nobel committee noted when it awarded the 1975 Prize in Medicine to both Baltimore and Temin, it began to erase the tenuous borders between viruses and genes.
Retroviruses cause cancers in chickens, sheep, mice, and other animals, but their effect on humans became clear only in the late nineteen-seventies, with the identification of two viruses that cause forms of leukemia. Retroviral proteins are particularly abundant in certain kinds of tumor cells, and scientists wondered to what degree they might be a cause of cancer. They were also curious about how retroviruses that infect us today differ from their ancestors. Working with mice in 2005, Thierry Heidmann found that endogenous retroviruses were present in large quantities in tumor cells. Similar viruses have been associated with many cancers (and other diseases). It is still not clear how they function, but they may help subvert the immune system, which would permit cancer cells to grow without restraint. Endogenous retroviruses also may actually protect us from viruses that are even worse. Experiments with mice and chickens have shown that they can block new infections by viruses with a similar genetic structure. Nonetheless, endogenous retroviruses are parasites, and in most cases the cells they infect would be better off without them. There is, however, one notable exception.
The earliest mammals, ancestors of the spiny anteater and the duck-billed platypus, laid eggs. Then, at least a hundred million years ago, embryos, instead of growing in a shell, essentially became parasites. While only balls of cells, they began to implant themselves in the lining of the womb. The result was the placenta, which permits the embyros to take nourishment from the mother's blood, while preventing immune cells or bacteria from entering. The placenta is essentially a modified egg. In the early nineteen-seventies, biologists who were scanning baboon placentas with an electron microscope were surprised to see retroviruses on a layer of tissue known as the syncytium, which forms the principal barrier between mother and fetus. They were even more surprised to see that all the animals were healthy. The same phenomenon was soon observed in mice, cats, guinea pigs, and humans. For many years, however, embryologists were not quite sure what to make of these placental discoveries. Most remained focussed on the potential harm a retrovirus could cause, rather than on any possible benefit. Cell fusion is a fundamental characteristic of the mammalian placenta but also, it turns out, of endogenous retroviruses. In fact, the protein syncytin, which causes placental cells to fuse together, employs the exact mechanism that enables retroviruses to latch on to the cells they infect.
The Nobel Prize-winning biologist Joshua Lederberg once wrote that the "single biggest threat to man's continued dominance on this planet is the virus." Harmit Malik, an evolutionary geneticist at the Fred Hutchinson Cancer Research Center, acknowledges the threat, yet he is confident that viruses may also provide one of our greatest scientific opportunities. Exploring that fundamental paradox - that our most talented parasites may also make us stronger - has become Malik's passion. "We have been in an evolutionary arms race with viruses for at least one hundred million years,'' he told me recently, when I visited his laboratory. "There is genetic conflict everywhere. You see it in processes that you would never suspect; in cell division, for instance, and in the production of proteins involved in the very essence of maintaining life.
"One party is winning and the other losing all the time," Malik went on. "That's evolution. It's the world's definitive game of cat and mouse. Viruses evolve, the host adapts, proteins change, viruses evade them. It never ends." The AIDS virus, for example, has one gene, called "vif," that does nothing but block a protein whose sole job is to stop the virus from making copies of itself. It simply takes that protein into the cellular equivalent of a trash can; if not for that gene, H.I.V. might have been a trivial disease. "To even think about the many million-year processes that caused that sort of evolution," Malik said, shaking his head in wonder. "It's dazzling." Malik grew up in Bombay and studied chemical engineering at the Indian Institute of Technology there, one of the most prestigious technical institutions in a country obsessed with producing engineers. He gave no real thought to biology, but he was wholly uninspired by his other studies. "It was fair to say I had little interest in chemical engineering, and I happened to tell that to my faculty adviser,'' he recalled. "He asked me what I liked. Well, I was reading Richard Dawkins at the time, his book 'The Selfish Gene' " - which asserts that a gene will operate in its own interest even if that means destroying an organism that it inhabits or helped create. The concept fascinated Malik. "I was thinking of becoming a philosopher,'' he said. "I thought I would study selfishness."
Malik's adviser had another idea. The university had just established a department of molecular biology, and Malik was dispatched to speak with its director. "This guy ended up teaching me by himself, sitting across the table. We met three times a week. I soon realized that he was testing out his course on me. I liked it and decided to apply to graduate school - although I had less than a tenth of the required biology courses. I had very little hope.'' But he had excellent test scores and in 1993 was accepted at the University of Rochester, as a graduate student in the biology department. He visited his new adviser as soon as he arrived. "He looked at my schedule and said, 'I see that you are doing genetics.' I had no clue what he was talking about, but I said sure, that sounds good. I had never taken a course in the subject. He gave me the textbook and told me that the class was for undergraduates, which made me feel more comfortable.'' It wasn't until the end of the conversation that Malik realized he would be teaching the class, not taking it.
The Hutchinson Center encourages its research scientists to collaborate with colleagues in seemingly unrelated fields. Malik and Michael Emerman, a virologist at the center's Human Biology and Basic Sciences Divisions, have been working together for four years. Malik's principal interest is historical: why did evolutionary pressures shape our defenses against viruses, and how have they done it? Emerman studies the genetic composition and molecular pathology of the AIDS virus. "Together, we are trying to understand what constellation of viruses we are susceptible to and why,'' Emerman told me. "We know at least that it is all a consequence of infections our ancestors had. So from there we want to try and derive a modern repertoire of antiviral genes."
They focussed on chimpanzees, our closest relatives. Chimpanzees are easily infected by the AIDS virus, but it never makes them sick. That has remained one of the most frustrating mysteries of the epidemic. How did nearly identical genetic relatives become immune to a virus that attacks us with such vigor? The most dramatic difference between the chimp genome and ours is that chimps have roughly a hundred and thirty copies of a virus called Pan troglodytes endogenous retrovirus, which scientists refer to by the acronym PtERV (pronounced "pea-terv"). Gorillas have eighty copies. Humans have none.
"We can see that PtERV infected gorillas and chimps four million years ago,'' Emerman told me. "But there was never any trace of its infecting humans." It is possible that all infected humans died, but it is far more likely that we developed a way to repel the virus. Nobody knew why until Emerman, Malik, and Shari Kaiser, a graduate student in Emerman's lab, presented evidence for a startling theory: the evolutionary process that protects us from PtERV may be the central reason we are vulnerable to H.I.V.
"We thought we must have a defense against this thing that they don't have,'' Malik told me, picking up the story the following day. Evolutionary biologists are not given to emotional outbursts - by definition, they take the long view. Malik is an engaging and voluble exception. When an antiviral protein excites him, he doesn't hold back. "Where but in evolutionary history can you see a story like this, with PtERV and the chimps?'' he asked, leaping up from his chair to begin sketching viral particles on a whiteboard. "It's simply amazing.''
He launched into a description of the complex interactions between viruses and the proteins that we have developed to fight them. There is one particular gene, called TRIM5a, that in humans manufactures a protein that binds to and destroys PtERV. "Our version of this gene is highly effective against PtERV, which is why we don't get infected,'' he said. Every primate has some version, but it works differently in each species - customized to fit the varying evolutionary requirements of each. In the rhesus monkey, that single gene provides complete protection against H.I.V. infection. In humans, it does nothing of the kind. "When Michael and I started to get into this business, people had never thought much about the evolutionary meaning of that gene. But we wondered, Is TRIM5a just an anti-H.I.V. factor or is there something else going on here?"
Like the two human retroviruses that were reconstructed in France and in New York, PtERV has long been extinct; Emerman and Malik realized that they would have to assemble a new version if they hoped to learn how we became immune to it. They took scores of viral sequences and lined them up to see what they had in common. The answer was almost everything. When there were differences in the sequence, the researchers used a statistical model to predict the most likely original version. Then they put the virus back together. (Like Bieniasz, in New York, they did so in such a way that the virus could reproduce only once.) They modified the human TRIM5a protein so that it would function like the chimp version. After that, the protein no longer protected humans against the reconstructed copy of the virus. Next, they tested this modified version against H.I.V. Emerman placed it in a dish, first with H.I.V. and next with PtERV. What he found astonished him. No matter how many times he repeated the test, the results never varied. "In every case, the protein blocked either PtERV or H.I.V.," Emerman told me. "But it never protected the cells from both viruses."
There are several possible ways to interpret the data, but the one favored by the researchers is that because humans developed an effective defense against one virus, PtERV, at about the time we split off from the chimps, five million years ago, we were left vulnerable to a new one, H.I.V. "If we can develop a drug that acts the same way the monkey version of this protein acts - so that it recognizes H.I.V. and neutralizes it - we could have a very effective therapy,'' Malik said. Both he and Emerman stressed that this day will not come soon. "First, we have to establish what part of TRIM5a is actually responsible for protecting monkeys against H.I.V.," Malik said. "Then we would have to try and make it as a drug" - and one that the human body won't reject. "The challenge is to find out how little you can change the human version and still make it effective against H.I.V. That is really what drives this whole story of re-creating that extinct virus and doing these experiments. Nobody is doing this as a gimmick. This virus could open doors that have been closed to us for millions of years. And if we can learn how to do that we have a chance to find a very effective response to one of the world's most incredibly effective viruses."
The Oxford University zoology department is housed in a forbidding concrete structure that looks like an Eastern European police station. The building is named for the Dutch ethologist Niko Tinbergen, whose work - with wasps and gulls, among other species - won him a Nobel Prize and helped establish the study of animal behavior as a science. Tinbergen's most famous student, Richard Dawkins, has carried on the university tradition of aggressive independence, and so have the younger members of the faculty. I stopped by the department a few months ago to have lunch with two of them, Aris Katzourakis and Robert Belshaw, both evolutionary biologists who have made the new field of paleovirology a specialty. Just before I arrived, Katzourakis had lobbed a bomb into the field.
Nobody knows what chain of evolutionary factors is required to transform an infectious virus - like H.I.V. - into one that is inherited. Such a virus would have to invade reproductive cells. H.I.V. doesn't do that. It belongs to a class called lentiviruses (from the Latin for "slow"), which are common in mammals like sheep and goats. Because lentiviruses had never been found in any animal's genome, most virologists assumed that they evolved recently. Until this summer, the oldest known lentivirus was "only" a million years, and almost no one thought that a lentivirus could become endogenous.
In a paper titled "Discovery and Analysis of the First Endogenous Lentivirus,'' published last spring in Proceedings of the National Academy of Sciences, Katzourakis, along with collaborators from Oxford, Stanford University, and Imperial College London, showed otherwise. They discovered the fossilized remains of an ancient lentivirus - the same type that causes AIDS - within the genome of the European rabbit (Oryctolagus cuniculus). "At first, I just assumed it was a mistake,'' Katzourakis told me over lunch in the building's cafeteria, Darwin's Café. "We checked it twice, three times. But we kept seeing genes that are found only in lentiviruses.'' They named their discovery "rabbit endogenous lentivirus type K," or RELIK. An obvious next step for Katzourakis and his group will be to work with virologists who can assemble a functional version of the ancient virus - as the researchers in Paris, New York, and Seattle have done. "It's the most promising way to explore the evolution and the impact of H.I.V.," he said.
It might be more than that. AIDS researchers have always been handicapped by the absence of a small-animal model in which to study the effects of the disease. It is not easy to use monkeys or sheep. They are expensive and difficult to obtain, and, for reasons of ethics, many experiments on them are proscribed. "Although RELIK is an ancient lentivirus and only defective copies were identified in this analysis,'' the authors wrote, "recent research has shown that it is possible to reconstruct infectious progenitors of such viruses," which, they concluded, could potentially "provide a small animal model for experimental research."
The discovery has already changed the way scientists think about viral evolution, and about H.I.V. in particular. "The most obvious implication is that we can no longer say that H.I.V. could not become endogenous,'' John Coffin, of Tufts, told me, though he still considers that unlikely. "It opens the field to a whole new level of examination." It also considerably alters the phylogenetic tree. RELIK is at least seven million years old, which makes it the oldest known lentivirus. "It is possible that primate lentiviruses such as H.I.V. and S.I.V.'' - its simian cousin - "are much older than people ever thought," Coffin said.
We can't be certain when endogenous retroviruses entered our genome, because it is impossible to watch a five-million-year process unfold. Yet in Australia a retrovirus seems to be evolving in front of our eyes. Beginning in the late nineteenth century, koalas on the mainland were hunted nearly to extinction. To protect them, as many as possible were captured and moved to several islands in the south. In the past hundred years, those koalas have been used to replenish the population on the mainland and on several other Australian islands. In many cases, though, they have become infected with a retrovirus that causes leukemia, immune disorders, and other diseases. It can even kill them. The epidemic presents a significant threat to the future of the species, and scientists have followed it closely. One group, from the University of Queensland, looked for the virus in koala DNA - and, as one would expect with a retrovirus, found it. The team also noticed that some of the babies, known as joeys, were infected in the same locations on their DNA as their parents. That means that the virus has become endogenous. Yet, when the scientists examined the koalas on Kangaroo Island, in the south, they discovered something they had not anticipated: none of the koalas were infected.
That could mean only one thing: since the infected animals had all been moved just in the past century, the koala retrovirus must have spread to Australia recently and is entering the genome now. That offers virologists and evolutionary biologists their first opportunity to learn how a virus transforms itself from something that can simply infect (and kill) its host to an organism that will become a permanent part of that host. Persistent viruses tend to grow weaker over the years. They couldn't live for long if they killed everything they infected. How they adapt, though, is a mystery. "Events like this have obviously occurred in human evolution,'' Paul Bieniasz told me - even with viruses like H.I.V. "We might be able to see how the koala infection settles into the genome, and whether it plays a role in helping its host fend off other viruses," he continued. "Whatever we learn will be useful, because we could never have learned it in any other way."
In 1963, Linus Pauling, the twentieth century's most influential chemist, wrote an essay, with Emile Zuckerkandl, in which they predicted that it would one day become possible to reconstruct extinct forms of life. It has taken half a century for scientists to acquire the information necessary to master most of the essential molecular biology and genetics, but there can no longer be any doubt that Pauling was right. Once you are able to assemble the ancestral sequence of any form of life, all you have to do is put the genes together, and back it comes.
"The knowledge you gain from resurrecting something that has not been alive for a million years has to be immensely valuable,'' Harmit Malik told me in Seattle. "We didn't take it lightly, and I don't think any of our colleagues did, either.'' He repeatedly pointed out that each virus was assembled in such a way that it could reproduce only once. "If you can't apply the knowledge, you shouldn't do the experiment," he said. Malik is a basic research scientist. His work is not directly related to drug development or treating disease. Still, he thinks deeply about the link between what he does and the benefits such work might produce. That is an entirely new way to look at the purpose of scientific research, which in the past was always propelled by intellectual curiosity, not utilitarian goals. Among élite scientists, it was usually considered gauche to be obsessed with anything so tangible or immediate; brilliant discoveries were supposed to percolate. But that paradigm was constructed before laboratories around the world got into the business of reshaping, resurrecting, and creating various forms of life.
The insights provided by recent advances in evolutionary biology have already been put to use, particularly in efforts to stop the AIDS virus. One of the main reasons that endogenous retroviruses can enter our genome without killing us is that they make many errors when they reproduce. Those errors are genetic mutations. The faster a cell reproduces (and the older it is), the more errors it is likely to make. And the more errors it makes the less likely it is to be dangerous to its host. "Viruses are accumulating and becoming more decrepit with every passing million years" was the way Malik described it to me. That realization has led AIDS researchers to contemplate a novel kind of drug. Until recently, antiviral medications had been designed largely to prevent H.I.V. from reproducing. Various drugs try to interfere with enzymes and other proteins that are essential for the virus to copy itself. There is a problem with this approach, however. Because the virus changes so rapidly, after a while a drug designed to stop it can lose its effectiveness completely. (That is why people take cocktails of H.I.V. medications; the combinations help slow the rate at which the virus learns to evade those interventions.)
Scientists at a company called Koronis Pharmaceuticals, just outside Seattle, are taking the opposite approach. They hope that by speeding up the life cycle of the AIDS virus they can drive it to extinction. The goal is to accelerate the virus's already rapid pace of mutation to the point where it produces such an enormous number of errors in its genome that it ceases to pose a threat. Like endogenous retroviruses, H.I.V. would become extinct. Earlier this month, researchers at the University of California at San Francisco and at the University of Toronto announced an even more fascinating way to use the fossils in our genome. H.I.V. infects immune-system cells and alters them so that they can produce more H.I.V. In doing so, they stimulate endogenous retroviruses, which then produce proteins that act as a sort of distress signal. Those signals can be detected on the surface of H.I.V.-infected cells, and in theory it should be possible to develop vaccines that target them. In essence, such a vaccine would act like a smart bomb, homing in on a signal transmitted from within each H.I.V.-infected cell. The team in San Francisco found strong evidence of those signals in the immune cells of fifteen of sixteen volunteers who were infected with H.I.V. In an uninfected control group, the signals were far weaker or were absent altogether. "For a vaccine against an infectious agent, this is a completely new strategy,'' Douglas Nixon, the immunologist who led the team, said. It's one that could not have emerged without the recent knowledge gained through experiments with endogenous retroviruses.
There may be no biological process more complicated than the relationships that viruses have with their hosts. Could it be that their persistence made it possible for humans to thrive? Luis P. Villarreal has posed that question many times, most notably in a 2004 essay, "Can Viruses Make Us Human?" Villarreal is the director of the Center for Virus Research at the University of California at Irvine. "This question will seem preposterous to most,'' his essay begins. "Viruses are molecular genetic parasites and are mostly recognized for their ability to induce disease." Yet he goes on to argue that they also represent "a major creative force'' in our evolution, driving each infected cell to acquire new and increasingly complex molecular identities. Villarreal was among the first to propose that endogenous retroviruses played a crucial role in the development of the mammalian placenta. He goes further than that, though: "Clearly, we have been observing evolution only for a very short time. Yet we can witness what current viruses," such as H.I.V., "can and might do to the human population."
Villarreal predicts that, without an effective AIDS vaccine, nearly the entire population of Africa will eventually perish. "We can also expect at least a few humans to survive,'' he wrote. They would be people who have been infected with H.I.V. yet, for some reason, do not get sick. "These survivors would thus be left to repopulate the continent. However, the resulting human population would be distinct" from those whom H.I.V. makes sick. These people would have acquired some combination of genes that confers resistance to H.I.V. There are already examples of specific mutations that seem to protect people against the virus. (For H.I.V. to infect immune cells, for example, it must normally dock with a receptor that sits on the surface of those cells. There are people, though, whose genes instruct them to build defective receptors. Those with two copies of that defect, one from each parent, are resistant to H.I.V. infection no matter how often they are exposed to the virus.) The process might take tens, or even hundreds, of thousands of years, but Darwinian selection would ultimately favor such mutations, and provide the opportunity for the evolution of a fitter human population. "If this were to be the outcome,'' Villarreal wrote, "we would see a new species of human, marked by its newly acquired endogenous viruses." The difference between us and this new species would be much like the difference that we know exists between humans and chimpanzees.
For Villarreal, and a growing number of like-minded scientists, the conclusion is clear. "Viruses may well be the unseen creator that most likely did contribute to making us human." ♦
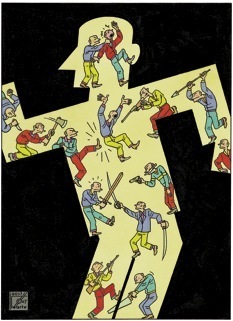
ILLUSTRATION: JOOST SWARTE


Reader Comments
to our Newsletter