
by Irving Kirsch
Basic Books, 226 pp., $15.99 (paper)
Anatomy of an Epidemic: Magic Bullets, Psychiatric Drugs, and the Astonishing Rise of Mental Illness in America
by Robert Whitaker
Crown, 404 pp., $26.00
Unhinged: The Trouble With Psychiatry - A Doctor's Revelations About a Profession in Crisis
by Daniel Carlat
Free Press, 256 pp., $25.00
It seems that Americans are in the midst of a raging epidemic of mental illness, at least as judged by the increase in the numbers treated for it. The tally of those who are so disabled by mental disorders that they qualify for Supplemental Security Income (SSI) or Social Security Disability Insurance (SSDI) increased nearly two and a half times between 1987 and 2007 - from one in 184 Americans to one in seventy-six. For children, the rise is even more startling - a thirty-five-fold increase in the same two decades. Mental illness is now the leading cause of disability in children, well ahead of physical disabilities like cerebral palsy or Down syndrome, for which the federal programs were created.
A large survey of randomly selected adults, sponsored by the National Institute of Mental Health (NIMH) and conducted between 2001 and 2003, found that an astonishing 46 percent met criteria established by the American Psychiatric Association (APA) for having had at least one mental illness within four broad categories at some time in their lives. The categories were "anxiety disorders," including, among other subcategories, phobias and post-traumatic stress disorder (PTSD); "mood disorders," including major depression and bipolar disorders; "impulse-control disorders," including various behavioral problems and attention-deficit/hyperactivity disorder (ADHD); and "substance use disorders," including alcohol and drug abuse. Most met criteria for more than one diagnosis. Of a subgroup affected within the previous year, a third were under treatment - up from a fifth in a similar survey ten years earlier.
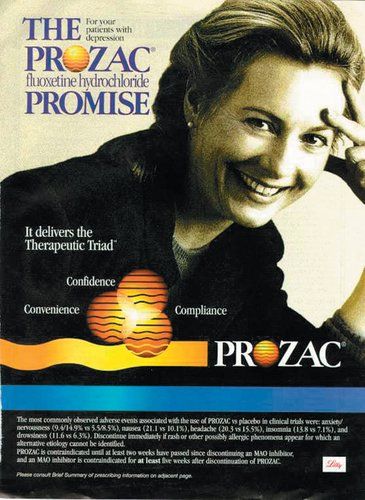
Nowadays treatment by medical doctors nearly always means psychoactive drugs, that is, drugs that affect the mental state. In fact, most psychiatrists treat only with drugs, and refer patients to psychologists or social workers if they believe psychotherapy is also warranted. The shift from "talk therapy" to drugs as the dominant mode of treatment coincides with the emergence over the past four decades of the theory that mental illness is caused primarily by chemical imbalances in the brain that can be corrected by specific drugs. That theory became broadly accepted, by the media and the public as well as by the medical profession, after Prozac came to market in 1987 and was intensively promoted as a corrective for a deficiency of serotonin in the brain. The number of people treated for depression tripled in the following ten years, and about 10 percent of Americans over age six now take antidepressants. The increased use of drugs to treat psychosis is even more dramatic. The new generation of antipsychotics, such as Risperdal, Zyprexa, and Seroquel, has replaced cholesterol-lowering agents as the top-selling class of drugs in the US.
What is going on here? Is the prevalence of mental illness really that high and still climbing? Particularly if these disorders are biologically determined and not a result of environmental influences, is it plausible to suppose that such an increase is real? Or are we learning to recognize and diagnose mental disorders that were always there? On the other hand, are we simply expanding the criteria for mental illness so that nearly everyone has one? And what about the drugs that are now the mainstay of treatment? Do they work? If they do, shouldn't we expect the prevalence of mental illness to be declining, not rising?
These are the questions, among others, that concern the authors of the three provocative books under review here. They come at the questions from different backgrounds - Irving Kirsch is a psychologist at the University of Hull in the UK, Robert Whitaker a journalist and previously the author of a history of the treatment of mental illness called Mad in America (2001), and Daniel Carlat a psychiatrist who practices in a Boston suburb and publishes a newsletter and blog about his profession.
The authors emphasize different aspects of the epidemic of mental illness. Kirsch is concerned with whether antidepressants work. Whitaker, who has written an angrier book, takes on the entire spectrum of mental illness and asks whether psychoactive drugs create worse problems than they solve. Carlat, who writes more in sorrow than in anger, looks mainly at how his profession has allied itself with, and is manipulated by, the pharmaceutical industry. But despite their differences, all three are in remarkable agreement on some important matters, and they have documented their views well.
First, they agree on the disturbing extent to which the companies that sell psychoactive drugs - through various forms of marketing, both legal and illegal, and what many people would describe as bribery - have come to determine what constitutes a mental illness and how the disorders should be diagnosed and treated. This is a subject to which I'll return.
Second, none of the three authors subscribes to the popular theory that mental illness is caused by a chemical imbalance in the brain. As Whitaker tells the story, that theory had its genesis shortly after psychoactive drugs were introduced in the 1950s. The first was Thorazine (chlorpromazine), which was launched in 1954 as a "major tranquilizer" and quickly found widespread use in mental hospitals to calm psychotic patients, mainly those with schizophrenia. Thorazine was followed the next year by Miltown (meprobamate), sold as a "minor tranquilizer" to treat anxiety in outpatients. And in 1957, Marsilid (iproniazid) came on the market as a "psychic energizer" to treat depression.
In the space of three short years, then, drugs had become available to treat what at that time were regarded as the three major categories of mental illness - psychosis, anxiety, and depression - and the face of psychiatry was totally transformed. These drugs, however, had not initially been developed to treat mental illness. They had been derived from drugs meant to treat infections, and were found only serendipitously to alter the mental state. At first, no one had any idea how they worked. They simply blunted disturbing mental symptoms. But over the next decade, researchers found that these drugs, and the newer psychoactive drugs that quickly followed, affected the levels of certain chemicals in the brain.
Some brief - and necessarily quite simplified - background: the brain contains billions of nerve cells, called neurons, arrayed in immensely complicated networks and communicating with one another constantly. The typical neuron has multiple filamentous extensions, one called an axon and the others called dendrites, through which it sends and receives signals from other neurons. For one neuron to communicate with another, however, the signal must be transmitted across the tiny space separating them, called a synapse. To accomplish that, the axon of the sending neuron releases a chemical, called a neurotransmitter, into the synapse. The neurotransmitter crosses the synapse and attaches to receptors on the second neuron, often a dendrite, thereby activating or inhibiting the receiving cell. Axons have multiple terminals, so each neuron has multiple synapses. Afterward, the neurotransmitter is either reabsorbed by the first neuron or metabolized by enzymes so that the status quo ante is restored. There are exceptions and variations to this story, but that is the usual way neurons communicate with one another.
When it was found that psychoactive drugs affect neurotransmitter levels in the brain, as evidenced mainly by the levels of their breakdown products in the spinal fluid, the theory arose that the cause of mental illness is an abnormality in the brain's concentration of these chemicals that is specifically countered by the appropriate drug. For example, because Thorazine was found to lower dopamine levels in the brain, it was postulated that psychoses like schizophrenia are caused by too much dopamine. Or later, because certain antidepressants increase levels of the neurotransmitter serotonin in the brain, it was postulated that depression is caused by too little serotonin. (These antidepressants, like Prozac or Celexa, are called selective serotonin reuptake inhibitors (SSRIs) because they prevent the reabsorption of serotonin by the neurons that release it, so that more remains in the synapses to activate other neurons.) Thus, instead of developing a drug to treat an abnormality, an abnormality was postulated to fit a drug.
That was a great leap in logic, as all three authors point out. It was entirely possible that drugs that affected neurotransmitter levels could relieve symptoms even if neurotransmitters had nothing to do with the illness in the first place (and even possible that they relieved symptoms through some other mode of action entirely). As Carlat puts it, "By this same logic one could argue that the cause of all pain conditions is a deficiency of opiates, since narcotic pain medications activate opiate receptors in the brain." Or similarly, one could argue that fevers are caused by too little aspirin.
But the main problem with the theory is that after decades of trying to prove it, researchers have still come up empty-handed. All three authors document the failure of scientists to find good evidence in its favor. Neurotransmitter function seems to be normal in people with mental illness before treatment. In Whitaker's words:
Prior to treatment, patients diagnosed with schizophrenia, depression, and other psychiatric disorders do not suffer from any known "chemical imbalance." However, once a person is put on a psychiatric medication, which, in one manner or another, throws a wrench into the usual mechanics of a neuronal pathway, his or her brain begins to function...abnormally.Carlat refers to the chemical imbalance theory as a "myth" (which he calls "convenient" because it destigmatizes mental illness), and Kirsch, whose book focuses on depression, sums up this way: "It now seems beyond question that the traditional account of depression as a chemical imbalance in the brain is simply wrong." Why the theory persists despite the lack of evidence is a subject I'll come to.
Do the drugs work? After all, regardless of the theory, that is the practical question. In his spare, remarkably engrossing book, The Emperor's New Drugs, Kirsch describes his fifteen-year scientific quest to answer that question about antidepressants. When he began his work in 1995, his main interest was in the effects of placebos. To study them, he and a colleague reviewed thirty-eight published clinical trials that compared various treatments for depression with placebos, or compared psychotherapy with no treatment. Most such trials last for six to eight weeks, and during that time, patients tend to improve somewhat even without any treatment. But Kirsch found that placebos were three times as effective as no treatment. That didn't particularly surprise him. What did surprise him was the fact that antidepressants were only marginally better than placebos. As judged by scales used to measure depression, placebos were 75 percent as effective as antidepressants. Kirsch then decided to repeat his study by examining a more complete and standardized data set.
The data he used were obtained from the US Food and Drug Administration (FDA) instead of the published literature. When drug companies seek approval from the FDA to market a new drug, they must submit to the agency all clinical trials they have sponsored. The trials are usually double-blind and placebo-controlled, that is, the participating patients are randomly assigned to either drug or placebo, and neither they nor their doctors know which they have been assigned. The patients are told only that they will receive an active drug or a placebo, and they are also told of any side effects they might experience. If two trials show that the drug is more effective than a placebo, the drug is generally approved. But companies may sponsor as many trials as they like, most of which could be negative - that is, fail to show effectiveness. All they need is two positive ones. (The results of trials of the same drug can differ for many reasons, including the way the trial is designed and conducted, its size, and the types of patients studied.)
For obvious reasons, drug companies make very sure that their positive studies are published in medical journals and doctors know about them, while the negative ones often languish unseen within the FDA, which regards them as proprietary and therefore confidential. This practice greatly biases the medical literature, medical education, and treatment decisions.
Kirsch and his colleagues used the Freedom of Information Act to obtain FDA reviews of all placebo-controlled clinical trials, whether positive or negative, submitted for the initial approval of the six most widely used antidepressant drugs approved between 1987 and 1999 - Prozac, Paxil, Zoloft, Celexa, Serzone, and Effexor. This was a better data set than the one used in his previous study, not only because it included negative studies but because the FDA sets uniform quality standards for the trials it reviews and not all of the published research in Kirsch's earlier study had been submitted to the FDA as part of a drug approval application.
Altogether, there were forty-two trials of the six drugs. Most of them were negative. Overall, placebos were 82 percent as effective as the drugs, as measured by the Hamilton Depression Scale (HAM-D), a widely used score of symptoms of depression. The average difference between drug and placebo was only 1.8 points on the HAM-D, a difference that, while statistically significant, was clinically meaningless. The results were much the same for all six drugs: they were all equally unimpressive. Yet because the positive studies were extensively publicized, while the negative ones were hidden, the public and the medical profession came to believe that these drugs were highly effective antidepressants.
Kirsch was also struck by another unexpected finding. In his earlier study and in work by others, he observed that even treatments that were not considered to be antidepressants - such as synthetic thyroid hormone, opiates, sedatives, stimulants, and some herbal remedies - were as effective as antidepressants in alleviating the symptoms of depression. Kirsch writes, "When administered as antidepressants, drugs that increase, decrease or have no effect on serotonin all relieve depression to about the same degree." What all these "effective" drugs had in common was that they produced side effects, which participating patients had been told they might experience.
It is important that clinical trials, particularly those dealing with subjective conditions like depression, remain double-blind, with neither patients nor doctors knowing whether or not they are getting a placebo. That prevents both patients and doctors from imagining improvements that are not there, something that is more likely if they believe the agent being administered is an active drug instead of a placebo. Faced with his findings that nearly any pill with side effects was slightly more effective in treating depression than an inert placebo, Kirsch speculated that the presence of side effects in individuals receiving drugs enabled them to guess correctly that they were getting active treatment - and this was borne out by interviews with patients and doctors - which made them more likely to report improvement. He suggests that the reason antidepressants appear to work better in relieving severe depression than in less severe cases is that patients with severe symptoms are likely to be on higher doses and therefore experience more side effects.
To further investigate whether side effects bias responses, Kirsch looked at some trials that employed "active" placebos instead of inert ones. An active placebo is one that itself produces side effects, such as atropine - a drug that selectively blocks the action of certain types of nerve fibers. Although not an antidepressant, atropine causes, among other things, a noticeably dry mouth. In trials using atropine as the placebo, there was no difference between the antidepressant and the active placebo. Everyone had side effects of one type or another, and everyone reported the same level of improvement. Kirsch reported a number of other odd findings in clinical trials of antidepressants, including the fact that there is no dose-response curve - that is, high doses worked no better than low ones - which is extremely unlikely for truly effective drugs. "Putting all this together," writes Kirsch,
"leads to the conclusion that the relatively small difference between drugs and placebos might not be a real drug effect at all. Instead, it might be an enhanced placebo effect, produced by the fact that some patients have broken [the] blind and have come to realize whether they were given drug or placebo. If this is the case, then there is no real antidepressant drug effect at all. Rather than comparing placebo to drug, we have been comparing "regular" placebos to "extra-strength" placebos."That is a startling conclusion that flies in the face of widely accepted medical opinion, but Kirsch reaches it in a careful, logical way. Psychiatrists who use antidepressants - and that's most of them - and patients who take them might insist that they know from clinical experience that the drugs work. But anecdotes are known to be a treacherous way to evaluate medical treatments, since they are so subject to bias; they can suggest hypotheses to be studied, but they cannot prove them. That is why the development of the double-blind, randomized, placebo-controlled clinical trial in the middle of the past century was such an important advance in medical science. Anecdotes about leeches or laetrile or megadoses of vitamin C, or any number of other popular treatments, could not stand up to the scrutiny of well-designed trials. Kirsch is a faithful proponent of the scientific method, and his voice therefore brings a welcome objectivity to a subject often swayed by anecdotes, emotions, or, as we will see, self-interest.
Whitaker's book is broader and more polemical. He considers all mental illness, not just depression. Whereas Kirsch concludes that antidepressants are probably no more effective than placebos, Whitaker concludes that they and most of the other psychoactive drugs are not only ineffective but harmful. He begins by observing that even as drug treatment for mental illness has skyrocketed, so has the prevalence of the conditions treated:
The number of disabled mentally ill has risen dramatically since 1955, and during the past two decades, a period when the prescribing of psychiatric medications has exploded, the number of adults and children disabled by mental illness has risen at a mind-boggling rate. Thus we arrive at an obvious question, even though it is heretical in kind: Could our drug-based paradigm of care, in some unforeseen way, be fueling this modern-day plague?Moreover, Whitaker contends, the natural history of mental illness has changed. Whereas conditions such as schizophrenia and depression were once mainly self-limited or episodic, with each episode usually lasting no more than six months and interspersed with long periods of normalcy, the conditions are now chronic and lifelong. Whitaker believes that this might be because drugs, even those that relieve symptoms in the short term, cause long-term mental harms that continue after the underlying illness would have naturally resolved.
The evidence he marshals for this theory varies in quality. He doesn't sufficiently acknowledge the difficulty of studying the natural history of any illness over a fifty-some-year time span during which many circumstances have changed, in addition to drug use. It is even more difficult to compare long-term outcomes in treated versus untreated patients, since treatment may be more likely in those with more severe disease at the outset. Nevertheless, Whitaker's evidence is suggestive, if not conclusive.
If psychoactive drugs do cause harm, as Whitaker contends, what is the mechanism? The answer, he believes, lies in their effects on neurotransmitters. It is well understood that psychoactive drugs disturb neurotransmitter function, even if that was not the cause of the illness in the first place. Whitaker describes a chain of effects. When, for example, an SSRI antidepressant like Celexa increases serotonin levels in synapses, it stimulates compensatory changes through a process called negative feedback. In response to the high levels of serotonin, the neurons that secrete it (presynaptic neurons) release less of it, and the postsynaptic neurons become desensitized to it. In effect, the brain is trying to nullify the drug's effects. The same is true for drugs that block neurotransmitters, except in reverse. For example, most antipsychotic drugs block dopamine, but the presynaptic neurons compensate by releasing more of it, and the postsynaptic neurons take it up more avidly. (This explanation is necessarily oversimplified, since many psychoactive drugs affect more than one of the many neurotransmitters.)
With long-term use of psychoactive drugs, the result is, in the words of Steve Hyman, a former director of the NIMH and until recently provost of Harvard University, "substantial and long-lasting alterations in neural function." As quoted by Whitaker, the brain, Hyman wrote, begins to function in a manner "qualitatively as well as quantitatively different from the normal state." After several weeks on psychoactive drugs, the brain's compensatory efforts begin to fail, and side effects emerge that reflect the mechanism of action of the drugs. For example, the SSRIs may cause episodes of mania, because of the excess of serotonin. Antipsychotics cause side effects that resemble Parkinson's disease, because of the depletion of dopamine (which is also depleted in Parkinson's disease). As side effects emerge, they are often treated by other drugs, and many patients end up on a cocktail of psychoactive drugs prescribed for a cocktail of diagnoses. The episodes of mania caused by antidepressants may lead to a new diagnosis of "bipolar disorder" and treatment with a "mood stabilizer," such as Depokote (an anticonvulsant) plus one of the newer antipsychotic drugs. And so on.
Some patients take as many as six psychoactive drugs daily. One well- respected researcher, Nancy Andreasen, and her colleagues published evidence that the use of antipsychotic drugs is associated with shrinkage of the brain, and that the effect is directly related to the dose and duration of treatment. As Andreasen explained to The New York Times, "The prefrontal cortex doesn't get the input it needs and is being shut down by drugs. That reduces the psychotic symptoms. It also causes the prefrontal cortex to slowly atrophy."*
Getting off the drugs is exceedingly difficult, according to Whitaker, because when they are withdrawn the compensatory mechanisms are left unopposed. When Celexa is withdrawn, serotonin levels fall precipitously because the presynaptic neurons are not releasing normal amounts and the postsynaptic neurons no longer have enough receptors for it. Similarly, when an antipsychotic is withdrawn, dopamine levels may skyrocket. The symptoms produced by withdrawing psychoactive drugs are often confused with relapses of the original disorder, which can lead psychiatrists to resume drug treatment, perhaps at higher doses.
Unlike the cool Kirsch, Whitaker is outraged by what he sees as an iatrogenic (i.e., inadvertent and medically introduced) epidemic of brain dysfunction, particularly that caused by the widespread use of the newer ("atypical") antipsychotics, such as Zyprexa, which cause serious side effects. Here is what he calls his "quick thought experiment":
Imagine that a virus suddenly appears in our society that makes people sleep twelve, fourteen hours a day. Those infected with it move about somewhat slowly and seem emotionally disengaged. Many gain huge amounts of weight - twenty, forty, sixty, and even one hundred pounds. Often their blood sugar levels soar, and so do their cholesterol levels. A number of those struck by the mysterious illness - including young children and teenagers - become diabetic in fairly short order.... The federal government gives hundreds of millions of dollars to scientists at the best universities to decipher the inner workings of this virus, and they report that the reason it causes such global dysfunction is that it blocks a multitude of neurotransmitter receptors in the brain - dopaminergic, serotonergic, muscarinic, adrenergic, and histaminergic. All of those neuronal pathways in the brain are compromised. Meanwhile, MRI studies find that over a period of several years, the virus shrinks the cerebral cortex, and this shrinkage is tied to cognitive decline. A terrified public clamors for a cure.If psychoactive drugs are useless, as Kirsch believes about antidepressants, or worse than useless, as Whitaker believes, why are they so widely prescribed by psychiatrists and regarded by the public and the profession as something akin to wonder drugs? Why is the current against which Kirsch and Whitaker and, as we will see, Carlat are swimming so powerful? I discuss these questions in Part II of this review.
Now such an illness has in fact hit millions of American children and adults. We have just described the effects of Eli Lilly's best-selling antipsychotic, Zyprexa.
Part II: The Illusions of Psychiatry1
In my article in the last issue, I focused mainly on the recent books by psychologist Irving Kirsch and journalist Robert Whitaker, and what they tell us about the epidemic of mental illness and the drugs used to treat it.1 Here I discuss the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM) - often referred to as the bible of psychiatry, and now heading for its fifth edition - and its extraordinary influence within American society. I also examine Unhinged, the recent book by Daniel Carlat, a psychiatrist, who provides a disillusioned insider's view of the psychiatric profession. And I discuss the widespread use of psychoactive drugs in children, and the baleful influence of the pharmaceutical industry on the practice of psychiatry.
One of the leaders of modern psychiatry, Leon Eisenberg, a professor at Johns Hopkins and then Harvard Medical School, who was among the first to study the effects of stimulants on attention deficit disorder in children, wrote that American psychiatry in the late twentieth century moved from a state of "brainlessness" to one of "mindlessness."2 By that he meant that before psychoactive drugs (drugs that affect the mental state) were introduced, the profession had little interest in neurotransmitters or any other aspect of the physical brain. Instead, it subscribed to the Freudian view that mental illness had its roots in unconscious conflicts, usually originating in childhood, that affected the mind as though it were separate from the brain.
But with the introduction of psychoactive drugs in the 1950s, and sharply accelerating in the 1980s, the focus shifted to the brain. Psychiatrists began to refer to themselves as psychopharmacologists, and they had less and less interest in exploring the life stories of their patients. Their main concern was to eliminate or reduce symptoms by treating sufferers with drugs that would alter brain function. An early advocate of this biological model of mental illness, Eisenberg in his later years became an outspoken critic of what he saw as the indiscriminate use of psychoactive drugs, driven largely by the machinations of the pharmaceutical industry.
When psychoactive drugs were first introduced, there was a brief period of optimism in the psychiatric profession, but by the 1970s, optimism gave way to a sense of threat. Serious side effects of the drugs were becoming apparent, and an antipsychiatry movement had taken root, as exemplified by the writings of Thomas Szasz and the movie One Flew Over the Cuckoo's Nest. There was also growing competition for patients from psychologists and social workers. In addition, psychiatrists were plagued by internal divisions: some embraced the new biological model, some still clung to the Freudian model, and a few saw mental illness as an essentially sane response to an insane world. Moreover, within the larger medical profession, psychiatrists were regarded as something like poor relations; even with their new drugs, they were seen as less scientific than other specialists, and their income was generally lower.
In the late 1970s, the psychiatric profession struck back - hard. As Robert Whitaker tells it in Anatomy of an Epidemic, the medical director of the American Psychiatric Association (APA), Melvin Sabshin, declared in 1977 that "a vigorous effort to remedicalize psychiatry should be strongly supported," and he launched an all-out media and public relations campaign to do exactly that. Psychiatry had a powerful weapon that its competitors lacked. Since psychiatrists must qualify as MDs, they have the legal authority to write prescriptions. By fully embracing the biological model of mental illness and the use of psychoactive drugs to treat it, psychiatry was able to relegate other mental health care providers to ancillary positions and also to identify itself as a scientific discipline along with the rest of the medical profession. Most important, by emphasizing drug treatment, psychiatry became the darling of the pharmaceutical industry, which soon made its gratitude tangible.
These efforts to enhance the status of psychiatry were undertaken deliberately. The APA was then working on the third edition of the DSM, which provides diagnostic criteria for all mental disorders. The president of the APA had appointed Robert Spitzer, a much-admired professor of psychiatry at Columbia University, to head the task force overseeing the project. The first two editions, published in 1952 and 1968, reflected the Freudian view of mental illness and were little known outside the profession. Spitzer set out to make the DSM-III something quite different. He promised that it would be "a defense of the medical model as applied to psychiatric problems," and the president of the APA in 1977, Jack Weinberg, said it would "clarify to anyone who may be in doubt that we regard psychiatry as a specialty of medicine."
When Spitzer's DSM-III was published in 1980, it contained 265 diagnoses (up from 182 in the previous edition), and it came into nearly universal use, not only by psychiatrists, but by insurance companies, hospitals, courts, prisons, schools, researchers, government agencies, and the rest of the medical profession. Its main goal was to bring consistency (usually referred to as "reliability") to psychiatric diagnosis, that is, to ensure that psychiatrists who saw the same patient would agree on the diagnosis. To do that, each diagnosis was defined by a list of symptoms, with numerical thresholds. For example, having at least five of nine particular symptoms got you a full-fledged diagnosis of a major depressive episode within the broad category of "mood disorders." But there was another goal - to justify the use of psychoactive drugs. The president of the APA last year, Carol Bernstein, in effect acknowledged that. "It became necessary in the 1970s," she wrote, "to facilitate diagnostic agreement among clinicians, scientists, and regulatory authorities given the need to match patients with newly emerging pharmacologic treatments."3
The DSM-III was almost certainly more "reliable" than the earlier versions, but reliability is not the same thing as validity. Reliability, as I have noted, is used to mean consistency; validity refers to correctness or soundness. If nearly all physicians agreed that freckles were a sign of cancer, the diagnosis would be "reliable," but not valid. The problem with the DSM is that in all of its editions, it has simply reflected the opinions of its writers, and in the case of the DSM-III mainly of Spitzer himself, who has been justly called one of the most influential psychiatrists of the twentieth century.4 In his words, he "picked everybody that [he] was comfortable with" to serve with him on the fifteen-member task force, and there were complaints that he called too few meetings and generally ran the process in a haphazard but high-handed manner. Spitzer said in a 1989 interview, "I could just get my way by sweet talking and whatnot." In a 1984 article entitled "The Disadvantages of DSM-III Outweigh Its Advantages," George Vaillant, a professor of psychiatry at Harvard Medical School, wrote that the DSM-III represented "a bold series of choices based on guess, taste, prejudice, and hope," which seems to be a fair description.
Not only did the DSM become the bible of psychiatry, but like the real Bible, it depended a lot on something akin to revelation. There are no citations of scientific studies to support its decisions. That is an astonishing omission, because in all medical publications, whether journal articles or textbooks, statements of fact are supposed to be supported by citations of published scientific studies. (There are four separate "sourcebooks" for the current edition of the DSM that present the rationale for some decisions, along with references, but that is not the same thing as specific references.) It may be of much interest for a group of experts to get together and offer their opinions, but unless these opinions can be buttressed by evidence, they do not warrant the extraordinary deference shown to the DSM. The DSM-III was supplanted by the DSM-III-R in 1987, the DSM-IV in 1994, and the current version, the DSM-IV-TR (text revised) in 2000, which contains 365 diagnoses. "With each subsequent edition," writes Daniel Carlat in his absorbing book, "the number of diagnostic categories multiplied, and the books became larger and more expensive. Each became a best seller for the APA, and DSM is now one of the major sources of income for the organization." The DSM-IV sold over a million copies.
As psychiatry became a drug-intensive specialty, the pharmaceutical industry was quick to see the advantages of forming an alliance with the psychiatric profession. Drug companies began to lavish attention and largesse on psychiatrists, both individually and collectively, directly and indirectly. They showered gifts and free samples on practicing psychiatrists, hired them as consultants and speakers, bought them meals, helped pay for them to attend conferences, and supplied them with "educational" materials. When Minnesota and Vermont implemented "sunshine laws" that require drug companies to report all payments to doctors, psychiatrists were found to receive more money than physicians in any other specialty. The pharmaceutical industry also subsidizes meetings of the APA and other psychiatric conferences. About a fifth of APA funding now comes from drug companies.
Drug companies are particularly eager to win over faculty psychiatrists at prestigious academic medical centers. Called "key opinion leaders" (KOLs) by the industry, these are the people who through their writing and teaching influence how mental illness will be diagnosed and treated. They also publish much of the clinical research on drugs and, most importantly, largely determine the content of the DSM. In a sense, they are the best sales force the industry could have, and are worth every cent spent on them. Of the 170 contributors to the current version of the DSM (the DSM-IV-TR), almost all of whom would be described as KOLs, ninety-five had financial ties to drug companies, including all of the contributors to the sections on mood disorders and schizophrenia.5
The drug industry, of course, supports other specialists and professional societies, too, but Carlat asks, "Why do psychiatrists consistently lead the pack of specialties when it comes to taking money from drug companies?" His answer: "Our diagnoses are subjective and expandable, and we have few rational reasons for choosing one treatment over another." Unlike the conditions treated in most other branches of medicine, there are no objective signs or tests for mental illness - no lab data or MRI findings - and the boundaries between normal and abnormal are often unclear. That makes it possible to expand diagnostic boundaries or even create new diagnoses, in ways that would be impossible, say, in a field like cardiology. And drug companies have every interest in inducing psychiatrists to do just that.
In addition to the money spent on the psychiatric profession directly, drug companies heavily support many related patient advocacy groups and educational organizations. Whitaker writes that in the first quarter of 2009 alone,
Eli Lilly gave $551,000 to NAMI [National Alliance on Mental Illness] and its local chapters, $465,000 to the National Mental Health Association, $130,000 to CHADD (an ADHD [attention deficit/hyperactivity disorder] patient-advocacy group), and $69,250 to the American Foundation for Suicide Prevention.And that's just one company in three months; one can imagine what the yearly total would be from all companies that make psychoactive drugs. These groups ostensibly exist to raise public awareness of psychiatric disorders, but they also have the effect of promoting the use of psychoactive drugs and influencing insurers to cover them. Whitaker summarizes the growth of industry influence after the publication of the DSM-III as follows:
In short, a powerful quartet of voices came together during the 1980's eager to inform the public that mental disorders were brain diseases. Pharmaceutical companies provided the financial muscle. The APA and psychiatrists at top medical schools conferred intellectual legitimacy upon the enterprise. The NIMH [National Institute of Mental Health] put the government's stamp of approval on the story. NAMI provided a moral authority.Like most other psychiatrists, Carlat treats his patients only with drugs, not talk therapy, and he is candid about the advantages of doing so. If he sees three patients an hour for psychopharmacology, he calculates, he earns about $180 per hour from insurers. In contrast, he would be able to see only one patient an hour for talk therapy, for which insurers would pay him less than $100. Carlat does not believe that psychopharmacology is particularly complicated, let alone precise, although the public is led to believe that it is:
Patients often view psychiatrists as wizards of neurotransmitters, who can choose just the right medication for whatever chemical imbalance is at play. This exaggerated conception of our capabilities has been encouraged by drug companies, by psychiatrists ourselves, and by our patients' understandable hopes for cures.His work consists of asking patients a series of questions about their symptoms to see whether they match up with any of the disorders in the DSM. This matching exercise, he writes, provides "the illusion that we understand our patients when all we are doing is assigning them labels." Often patients meet criteria for more than one diagnosis, because there is overlap in symptoms. For example, difficulty concentrating is a criterion for more than one disorder. One of Carlat's patients ended up with seven separate diagnoses. "We target discrete symptoms with treatments, and other drugs are piled on top to treat side effects." A typical patient, he says, might be taking Celexa for depression, Ativan for anxiety, Ambien for insomnia, Provigil for fatigue (a side effect of Celexa), and Viagra for impotence (another side effect of Celexa).
As for the medications themselves, Carlat writes that "there are only a handful of umbrella categories of psychotropic drugs," within which the drugs are not very different from one another. He doesn't believe there is much basis for choosing among them. "To a remarkable degree, our choice of medications is subjective, even random. Perhaps your psychiatrist is in a Lexapro mood this morning, because he was just visited by an attractive Lexapro drug rep." And he sums up:
Such is modern psychopharmacology. Guided purely by symptoms, we try different drugs, with no real conception of what we are trying to fix, or of how the drugs are working. I am perpetually astonished that we are so effective for so many patients.While Carlat believes that psychoactive drugs are sometimes effective, his evidence is anecdotal. What he objects to is their overuse and what he calls the "frenzy of psychiatric diagnoses." As he puts it, "if you ask any psychiatrist in clinical practice, including me, whether antidepressants work for their patients, you will hear an unambiguous 'yes.' We see people getting better all the time." But then he goes on to speculate, like Irving Kirsch in The Emperor's New Drugs, that what they are really responding to could be an activated placebo effect. If psychoactive drugs are not all they're cracked up to be - and the evidence is that they're not - what about the diagnoses themselves? As they multiply with each edition of the DSM, what are we to make of them?
In 1999, the APA began work on its fifth revision of the DSM, which is scheduled to be published in 2013. The twenty-seven-member task force is headed by David Kupfer, a professor of psychiatry at the University of Pittsburgh, assisted by Darrel Regier of the APA's American Psychiatric Institute for Research and Education. As with the earlier editions, the task force is advised by multiple work groups, which now total some 140 members, corresponding to the major diagnostic categories. Ongoing deliberations and proposals have been extensively reported on the APA website (www.DSM5.org) and in the media, and it appears that the already very large constellation of mental disorders will grow still larger.
In particular, diagnostic boundaries will be broadened to include precursors of disorders, such as "psychosis risk syndrome" and "mild cognitive impairment" (possible early Alzheimer's disease). The term "spectrum" is used to widen categories, for example, "obsessive-compulsive disorder spectrum," "schizophrenia spectrum disorder," and "autism spectrum disorder." And there are proposals for entirely new entries, such as "hypersexual disorder," "restless legs syndrome," and "binge eating."
Even Allen Frances, chairman of the DSM-IV task force, is highly critical of the expansion of diagnoses in the DSM-V. In the June 26, 2009, issue of Psychiatric Times, he wrote that the DSM-V will be a "bonanza for the pharmaceutical industry but at a huge cost to the new false positive patients caught in the excessively wide DSM-V net." As if to underscore that judgment, Kupfer and Regier wrote in a recent article in the Journal of the American Medical Association (JAMA), entitled "Why All of Medicine Should Care About DSM-5," that "in primary care settings, approximately 30 percent to 50 percent of patients have prominent mental health symptoms or identifiable mental disorders, which have significant adverse consequences if left untreated."6 It looks as though it will be harder and harder to be normal.
At the end of the article by Kupfer and Regier is a small-print "financial disclosure" that reads in part:
Prior to being appointed as chair, DSM-5 Task Force, Dr. Kupfer reports having served on advisory boards for Eli Lilly & Co, Forest Pharmaceuticals Inc, Solvay/Wyeth Pharmaceuticals, and Johnson & Johnson; and consulting for Servier and Lundbeck.Regier oversees all industry-sponsored research grants for the APA. The DSM-V (used interchangeably with DSM-5) is the first edition to establish rules to limit financial conflicts of interest in members of the task force and work groups. According to these rules, once members were appointed, which occurred in 2006 - 2008, they could receive no more than $10,000 per year in aggregate from drug companies or own more than $50,000 in company stock. The website shows their company ties for three years before their appointments, and that is what Kupfer disclosed in the JAMA article and what is shown on the APA website, where 56 percent of members of the work groups disclosed significant industry interests.
The pharmaceutical industry influences psychiatrists to prescribe psychoactive drugs even for categories of patients in whom the drugs have not been found safe and effective. What should be of greatest concern for Americans is the astonishing rise in the diagnosis and treatment of mental illness in children, sometimes as young as two years old. These children are often treated with drugs that were never approved by the FDA for use in this age group and have serious side effects. The apparent prevalence of "juvenile bipolar disorder" jumped forty-fold between 1993 and 2004, and that of "autism" increased from one in five hundred children to one in ninety over the same decade. Ten percent of ten-year-old boys now take daily stimulants for ADHD - "attention deficit/hyperactivity disorder" - and 500,000 children take antipsychotic drugs.
There seem to be fashions in childhood psychiatric diagnoses, with one disorder giving way to the next. At first, ADHD, manifested by hyperactivity, inattentiveness, and impulsivity usually in school-age children, was the fastest-growing diagnosis. But in the mid-1990s, two highly influential psychiatrists at the Massachusetts General Hospital proposed that many children with ADHD really had bipolar disorder that could sometimes be diagnosed as early as infancy. They proposed that the manic episodes characteristic of bipolar disorder in adults might be manifested in children as irritability. That gave rise to a flood of diagnoses of juvenile bipolar disorder. Eventually this created something of a backlash, and the DSM-V now proposes partly to replace the diagnosis with a brand-new one, called "temper dysregulation disorder with dysphoria," or TDD, which Allen Frances calls "a new monster."7
One would be hard pressed to find a two-year-old who is not sometimes irritable, a boy in fifth grade who is not sometimes inattentive, or a girl in middle school who is not anxious. (Imagine what taking a drug that causes obesity would do to such a girl.) Whether such children are labeled as having a mental disorder and treated with prescription drugs depends a lot on who they are and the pressures their parents face.8 As low-income families experience growing economic hardship, many are finding that applying for Supplemental Security Income (SSI) payments on the basis of mental disability is the only way to survive. It is more generous than welfare, and it virtually ensures that the family will also qualify for Medicaid. According to MIT economics professor David Autor, "This has become the new welfare." Hospitals and state welfare agencies also have incentives to encourage uninsured families to apply for SSI payments, since hospitals will get paid and states will save money by shifting welfare costs to the federal government.
Growing numbers of for-profit firms specialize in helping poor families apply for SSI benefits. But to qualify nearly always requires that applicants, including children, be taking psychoactive drugs. According to a New York Times story, a Rutgers University study found that children from low-income families are four times as likely as privately insured children to receive antipsychotic medicines.
In December 2006 a four-year-old child named Rebecca Riley died in a small town near Boston from a combination of Clonidine and Depakote, which she had been prescribed, along with Seroquel, to treat "ADHD" and "bipolar disorder" - diagnoses she received when she was two years old. Clonidine was approved by the FDA for treating high blood pressure. Depakote was approved for treating epilepsy and acute mania in bipolar disorder. Seroquel was approved for treating schizophrenia and acute mania. None of the three was approved to treat ADHD or for long-term use in bipolar disorder, and none was approved for children Rebecca's age. Rebecca's two older siblings had been given the same diagnoses and were each taking three psychoactive drugs. The parents had obtained SSI benefits for the siblings and for themselves, and were applying for benefits for Rebecca when she died. The family's total income from SSI was about $30,000 per year.9
Whether these drugs should ever have been prescribed for Rebecca in the first place is the crucial question. The FDA approves drugs only for specified uses, and it is illegal for companies to market them for any other purpose - that is, "off-label." Nevertheless, physicians are permitted to prescribe drugs for any reason they choose, and one of the most lucrative things drug companies can do is persuade physicians to prescribe drugs off-label, despite the law against it. In just the past four years, five firms have admitted to federal charges of illegally marketing psychoactive drugs. AstraZeneca marketed Seroquel off-label for children and the elderly (another vulnerable population, often administered antipsychotics in nursing homes); Pfizer faced similar charges for Geodon (an antipsychotic); Eli Lilly for Zyprexa (an antipsychotic); Bristol-Myers Squibb for Abilify (another antipsychotic); and Forest Labs for Celexa (an antidepressant).
Despite having to pay hundreds of millions of dollars to settle the charges, the companies have probably come out well ahead. The original purpose of permitting doctors to prescribe drugs off-label was to enable them to treat patients on the basis of early scientific reports, without having to wait for FDA approval. But that sensible rationale has become a marketing tool. Because of the subjective nature of psychiatric diagnosis, the ease with which diagnostic boundaries can be expanded, the seriousness of the side effects of psychoactive drugs, and the pervasive influence of their manufacturers, I believe doctors should be prohibited from prescribing psychoactive drugs off-label, just as companies are prohibited from marketing them off-label.
The books by Irving Kirsch, Robert Whitaker, and Daniel Carlat are powerful indictments of the way psychiatry is now practiced. They document the "frenzy" of diagnosis, the overuse of drugs with sometimes devastating side effects, and widespread conflicts of interest. Critics of these books might argue, as Nancy Andreasen implied in her paper on the loss of brain tissue with long-term antipsychotic treatment, that the side effects are the price that must be paid to relieve the suffering caused by mental illness. If we knew that the benefits of psychoactive drugs outweighed their harms, that would be a strong argument, since there is no doubt that many people suffer grievously from mental illness. But as Kirsch, Whitaker, and Carlat argue convincingly, that expectation may be wrong.
At the very least, we need to stop thinking of psychoactive drugs as the best, and often the only, treatment for mental illness or emotional distress. Both psychotherapy and exercise have been shown to be as effective as drugs for depression, and their effects are longer-lasting, but unfortunately, there is no industry to push these alternatives and Americans have come to believe that pills must be more potent. More research is needed to study alternatives to psychoactive drugs, and the results should be included in medical education.
Comment: In addition to psychotherapy and exercise as alternatives to psychiatric drugs, we could add dietary changes (eliminating gluten grains, dairy products, and industrial oils, for example) and breathing/meditation programs such as Éiriú Eolas.
In particular, we need to rethink the care of troubled children. Here the problem is often troubled families in troubled circumstances. Treatment directed at these environmental conditions - such as one-on-one tutoring to help parents cope or after-school centers for the children - should be studied and compared with drug treatment. In the long run, such alternatives would probably be less expensive. Our reliance on psychoactive drugs, seemingly for all of life's discontents, tends to close off other options. In view of the risks and questionable long-term effectiveness of drugs, we need to do better. Above all, we should remember the time-honored medical dictum: first, do no harm (primum non nocere).
1. See Marcia Angell, " The Epidemic of Mental Illness: Why? ," The New York Review, June 23, 2011.
2. Eisenberg wrote about this transition in "Mindlessness and Brainlessness," British Journal of Psychiatry, No. 148 (1986). His last paper, completed by his stepson, was published after his death in 2009. See Eisenberg and L.B. Guttmacher, "Were We All Asleep at the Switch? A Personal Reminiscence of Psychiatry from 1940 to 2010," Acta Psychiatrica Scand, No. 122 (2010).
3. Carol A. Bernstein, "Meta-Structure in DSM-5 Process," Psychiatric News, March 4, 2011, p. 7.
4. The history of the DSM is recounted in Christopher Lane's informative book Shyness: How Normal Behavior Became a Sickness (Yale University Press, 2007). Lane was given access to the American Psychiatric Association's archive of unpublished letters, transcripts, and memoranda, and he also interviewed Robert Spitzer. His book was reviewed by Frederick Crews in The New York Review , December 6, 2007 , and by me, January 15, 2009 .
5. See L. Cosgrove et al., "Financial Ties Between DSM-IV Panel Members and the Pharmaceutical Industry," Psychotherapy and Psychosomatics, Vol. 75 (2006).
6. David J. Kupfer and Darrel A. Regier, "Why All of Medicine Should Care About DSM-5," JAMA, May 19, 2010.
7. Greg Miller, "Anything But Child's Play," Science, March 5, 2010.
8. Duff Wilson, "Child's Ordeal Reveals Risks of Psychiatric Drugs in Young," The New York Times, September 2, 2010.
9. Patricia Wen, "A Legacy of Unintended Side-Effects: Call It the Other Welfare," The Boston Globe, December 12, 2010.


The story of poor Rebecca Riley is heartbreaking. Being fed three dangerous drugs at the age of four? She was not mentally ill, but the people who sanctioned that dispensation most definitely are.
But they are no doubt still alive, and she is dead. The blind bastards.
I am sick to death of pill pushing "experts", who are little other than trendies, they'll follow whatever prevailing wind comes along. That kind of naivety is more akin to mental illness than many of the conditions noted on the DSM, I reckon.