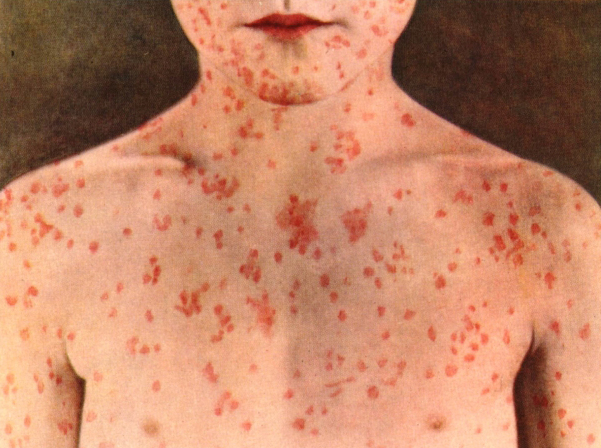
In the 1960s, a measles vaccine was introduced. During the next several years, cases of the disease declined. However, a significant reduction in the severity of measles occurred long before the vaccine was introduced. For example, in 1900 there were 13.3 measles deaths in the United States per 100,000 people. By 1955 -- eight years before the first measles vaccine became available - the death rate had declined on its own by 97.7% to .03 deaths per 100,000.(1) Data published in International Mortality Statistics shows that from 1915 to 1958 the measles death rate in the United States and United Kingdom declined by 98%.(2)
Eradication of Measles
When the measles vaccine was introduced in 1963, health officials were confident that they could eradicate the disease by 1967.(3) That did not occur. In 1978, the federal government announced its new goal to eradicate measles from the U.S. by 1982.(4) That did not occur. In 1994, health authorities once again targeted measles for elimination from the Western Hemisphere by the year 2000.(5) Although the CDC officially declared that measles was eliminated in 2000, outbreaks continue to occur.
According to the CDC, as of June 27 of this year there were 539 cases of measles in the United States, out of a population of more than 318 million.(6) That is a very tiny number. The last time that somebody died from measles in the United States was 11 years ago.(7)
What is causing these small outbreaks of measles? According to authorities, decreasing vaccination rates are responsible. However, vaccine coverage rates in the United States have remained high and stable since 1996. According to the World Health Organization (WHO), every year for the past 17 years, about 92% of all 1-year-olds eligible for a measles vaccine (MMR) have been vaccinated.(8) Thus, if measles cases are on the rise, it cannot be blamed on decreasing vaccination rates.
Authorities also claim that unvaccinated people are contracting the disease and spreading it to others. However, a study published this year in Clinical Infectious Diseases showed that people who are fully vaccinated against measles can spread the disease to other people who are fully vaccinated against measles. Thus, vaccinated people are vectors for the disease.(9)
Another problem with the measles vaccine is that it may be technologically archaic, inadequate for the 21st century, out of alignment with current scientific knowledge about how the immune system operates. It was made to be given with a "one dose fits all" approach. It assumes that everyone is at equal risk of complications from disease and that their immune responses to the vaccine will be similar. However, a recent study confirmed that when healthy children are vaccinated against measles there is a wide variation in their antibody levels. The diversity of these inter-individual antibody responses may determine whether the vaccine is protective or ineffective when the vaccinated person is challenged by the disease.(10)
It is also important to note that in nearly every outbreak of measles, large percentages of the cases occur in people who were fully vaccinated against the disease. For example, in 1988, 69% of all school-aged children in the U.S. who contracted measles were adequately vaccinated.(11) In 1995, 56% of all measles cases in the U.S. occurred in people who were previously vaccinated.(12)
There are several possible reasons to explain why fully vaccinated people are still susceptible to contracting measles. Two of these reasons were already discussed: 1) people who are fully vaccinated against measles can spread the disease to other people who are fully vaccinated against measles, and 2) some vaccinated people will not develop protective antibody levels.
Vaccine failures also occur because of decreasing immunity over time. When the measles vaccine was introduced, authorities promised everyone that one dose would protect for life. But immunity from vaccination is temporary, the reason a booster dose was added to the vaccine schedule - to compensate for the short‑lived boost in antibody production from just one shot. High antibody levels gained through vaccination decline after several years, unlike natural immunity which provides lifelong protection against the disease.
It is also important to understand that artificial immunity conferred through vaccination may be stimulated by regular contact with the natural disease. This is known as exogenous boosting. However, due to widespread measles vaccination, circulation of the natural measles virus is rare, lowering opportunities for boosting immunity among vaccinated persons. Scientists believe that this may contribute to waning antibody levels, loss of population immunity to measles, and an increased ability of vaccinated persons to contract and transmit the disease.(9)
Herd Immunity
In 1933, A.W. Hedrich published a study on epidemiological patterns of measles. He concluded that when 68 percent of children less than 15 years of age are immune to the disease, epidemics do not develop.(13) Authorities retained this general idea - that a precise degree of herd immunity will prevent epidemics - but remain unclear about the level required to achieve it.
In 1991, the CDC concluded that measles outbreaks can be avoided if 70 to 80 percent of two‑year olds in inner cities are vaccinated.(14) A 1992 study published in the Journal of the American Medical Association also concluded that the "immunization coverage of two‑year olds of 80 percent or less may be sufficient to prevent sustained measles outbreaks in urban communities."(15)
Today, authorities concede that earlier guesses about herd immunity were wrong. Greater than 90% of all eligible children in the U.S. have been vaccinated against measles yet outbreaks continue to occur. Even two doses of the measles vaccine are insufficient to achieve the elusive herd immunity and authorities are now demanding that nearly everyone must be vaccinated or the people who are vaccinated won't be protected!
Despite extensive evidence showing several problems with the current measles vaccine and measles vaccination strategies, health authorities blame unvaccinated people for outbreaks of disease in vaccinated populations. They instigate irrational fear in the parents of vaccinated children and animosity between vaccinated and unvaccinated families.
Overzealous pro-vaccinators believe that the vaccine is ineffective in those who receive it unless the small percentage of unvaccinated people submit to compulsory vaccination as well. When authorities claim that vaccinated people are at risk of getting measles if some people are permitted to remain unvaccinated, they are essentially arguing that the small number of unvaccinated people are responsible for safeguarding vaccinated populations - the UN-vaccinated are key to whether the vaccinated are truly protected!
Authorities also claim that vaccinated people protect the unvaccinated AND that the unvaccinated are at risk of getting the disease. So the unvaccinated are protected and unprotected at the same time! (Schrodinger and his paradoxical cat would love this argument.)
Food and Nutritional Supplementation
Although measles is rarely a dangerous disease in developed nations where proper nutrition and access to healthcare are available, in third world nations where pregnant mothers and their babies are malnourished, measles can be a serious disease. However, a measles vaccine may not be sufficient to protect children from excess morbidity and mortality.
Today, most developing nations require their infants to receive several inoculations, including a measles vaccine at 9 months of age. They have very high vaccine coverage rates (a percentage of the target population that has been vaccinated), yet their infant mortality rates are dreadfully unacceptable. For example, in 2011, Gambia, a poor country in Africa, required its infants to receive multiple vaccines, vaccinated 90% to 96% of its infants (91% received measles vaccines), yet 58 of every 1000 infants still died before their first birthdays. Ghana also required its infants to receive several vaccines, vaccinated 91% to 98% of its infants (91% received measles vaccines) yet also had a dismal infant mortality rate: 52 of every 1000 infants died before their first birthdays.(16)
These examples appear to confirm that high vaccination rates are not sufficient to reduce complications and deaths from measles and other causes. Clean water, proper nutrition, good sanitation, and easy access to health care are the most important factors to improve infant mortality rates in unclean, poorly nourished, and impoverished areas of the world.(17-19)
Malnutrition is a global problem and may be the most significant factor requiring immediate attention. It has been linked with a diminished immune function. A weakened immune system often results in an increased susceptibility to infections.(18) Even mild infections have adverse effects on nutritional status. Conversely, almost any nutritional deficiency will lower resistance to disease.
The importance of proper nutrition cannot be overemphasized. For example, several studies have shown that high doses of vitamin A are protective against complications and deaths from measles. A recent paper published by the International Journal of Epidemiology found that vitamin A treatment for measles recommended by the World Health Organization reduced measles mortality by 62%.(20) A randomized clinical trial published in the British Medical Journal found that the death rate in children under 2 years of age declined by 87% in the group that received vitamin A supplementation when compared to the group that only received routine treatment.(21)
Pregnant women and children living in third world nations need to be provided with healthy, nutritious food and supplemented with all the vitamins and nutrients required for building strong bodies and robust immune systems. There are many reasons why outbreaks of measles continue to occur in both developed and developing nations. By refocusing our efforts on addressing archaic vaccination policies while eliminating hunger and malnourishment, childhood challenges from infectious diseases do not have to invoke anxiety and fear. Some infections might even provide advantages. For example, studies confirm that women who contracted measles or mumps in childhood are significantly less likely to develop ovarian cancer as adults.(22,23)
Misplaced Priorities
Considering the evidence presented in this paper, perhaps the CDC and other health authorities should stop provoking inordinate concern over 539 cases of measles in the United States out of a population of more than 318 million - 1 case, no deaths, per every 590,000 citizens - and should focus instead on a rising epidemic of type 1 diabetes that has been scientifically linked to vaccinations (24,25) or aluminum adjuvants in vaccines that have been scientifically linked to autoimmune and neurological disorders.(26-29)
Our health authorities could also bring attention to the serious problem of malnutrition in our own great nation. In 2010 (the most recent year with complete figures) 2,948 people died from nutritional deficiencies.(30) Why is there manufactured outrage over 539 cases of measles (no deaths) in the United States but complete silence over nearly 3,000 American deaths annually from nutritional deficiencies?
The FDA, CDC, WHO, and other overzealous pro-vaccinators need to back off from their "one dose fits all" technologically archaic vaccination policies and stop blaming non-vaccinators for vaccine failures. If you take an aspirin to ward off a headache and you still feel a throbbing pain, the aspirin didn't work. It failed. The manufacturer made an inferior product. Your headache was not caused by everyone else nearby who refused to take an aspirin. That's ridiculous.
The measles vaccine also poses significant risks of irreversible harm, including the potential for blood disorders, sensory impairments, immune system suppression, brain damage and death. These possibilities are well documented in the medical literature and manufacturer's product inserts.(31) Therefore, no one should be intimidated or coerced into vaccinating against their will. Parents must remain free to accept or reject vaccines for their children.
In summary:
- A significant reduction in the severity of measles occurred long before the vaccine was introduced.
- Measles vaccination rates are not declining. They have remained stable and high for the past 17 years.
- People who are fully vaccinated against measles can spread the disease to other people who are fully vaccinated against measles.
- The measles vaccine may be technologically archaic, causing a wide variation in eliciting either protective or ineffective antibody levels.
- In nearly every outbreak of measles, a large percentage of cases occur in people who were fully vaccinated against the disease.
- High antibody levels gained through vaccination decline after several years, unlike natural immunity which provides lifelong protection against the disease.
- Due to widespread measles vaccination, circulation of the natural measles virus is rare, lowering opportunities for boosting immunity among vaccinated persons. This may contribute to waning antibody levels, loss of population immunity to measles, and an increased ability of vaccinated persons to contract and transmit the disease.
- High vaccination rates and two doses of a measles vaccine are insufficient to achieve the elusive herd immunity.
- Health authorities blame a small number of unvaccinated people for outbreaks of disease in vaccinated populations, essentially arguing that the UN-vaccinated are key to whether the vaccinated are truly protected.
- Authorities claim that vaccinated people protect the unvaccinated AND that the unvaccinated are at risk of getting the disease -- they are protected and unprotected at the same time.
- In third world nations where pregnant mothers and their babies are malnourished, measles can be a serious disease.
- In third world nations without clean water, proper nutrition, good sanitation, and easy access to health care, high vaccination rates may be insufficient to reduce complications and deaths from measles and other causes.
- Malnutrition is a global problem that can lead to nutritional deficiencies lowering resistance to disease.
- High doses of vitamin A are protective against complications and deaths from measles.
- Pregnant women and children living in third world nations need to be provided with healthy, nutritious food and supplemented with all the vitamins and nutrients required for building strong bodies and robust immune systems.
- Health authorities should stop manufacturing inordinate concern over a relatively small number or measles cases and should focus instead on epidemics of diabetes, autoimmune and neurological disorders that have been scientifically linked to vaccinations.
- Health authorities in the U.S. have instigated outrage over 539 cases of measles but remain silent over nearly 3,000 American deaths annually from nutritional deficiencies.
- If you take a pill or drug for a particular health condition and it doesn't work, then it failed. It would be absurd to blame your neighbors. The manufacturer made an inferior product.
- The measles vaccine poses significant risks of irreversible harm.
- No one should be intimidated or coerced into vaccinating against their will. Parents must remain free to accept or reject vaccines for their children.
1. Mendelsohn R. How to Raise a Healthy Child...In Spite of Your Doctor. (Ballantine Books, 1987): 237.
2. Alderson M. International Mortality Statistics (Washington, DC: Facts on File, 1981): 182-83.
3. Sencer DJ, et al. Epidemiological basis for eradication of measles in 1967. Public Health Report 1967; 82: 253-61.
4. Hinman AR. The opportunity and obligation to eliminate measles from the United States. Journal of the American Medical Association 1979; 242(11): 1157-62.
5. Neuzil KM. Eradication of polio, measles, and hib. Third Annual Conference on Vaccine Research 2000.
6. CDC. Measles cases and outbreaks, January 1 to June 27, 2014.
7. U.S. health officials report spike in measles cases. The Washington Post 2013 December 5. www.washingtonpost.com
8. WHO. Immunization surveillance, assessment and monitoring. Measles (MCV) immunization coverage among 1-year-olds, 1980-2012 (%): 2012.
9. Rosen JB, Rota JS, et al. Outbreak of measles among persons with prior evidence of immunity, New York City, 2011. Clin Infect Dis 2014 May; 58(9): 1205-10.
10. Poland GA, Kennedy RB, et al. Vaccinomics and personalized vaccinology: is science leading us toward a new path of directed vaccine development and discovery? PloS Pathog 2011 Dec; 7(12): e1002344.
11. CDC. Measles. MMWR 1989; 38: 329-30.
12. Gold E. Current progress in measles eradication in the U.S. Infect Med 1997; 14(4): 297-310.
13. Cherry JD. The 'new' epidemiology of measles and rubella. Hospital Practice 1980 July: 53-54.
14. CDC. Measles vaccination levels among selected groups of preschool-aged children -- USA. MMWR 1991; 40: 36-39.
15. Schlenker TL, et al. Measles herd immunity: the association of attack rats with immunization rates in preschool children. JAMA 1992; 267(6): 826.
16. WHO/UNICEF. Immunization Summary: A Statistical Reference Containing Data Through 2011 (The 2013 Edition).
17. Wegman ME. Infant mortality in the 20th century, dramatic but uneven progress. J Nutr 2001; 131: 401SB408S.
18. Beck MA. The role of nutrition in viral disease. J Nutri Biochem 1996; 7: 683B690.
19. Scrimshaw NS and SanGiovanni JP. Synergism of nutrition, infection, and immunity: an overview. Am J Clin Nutr 1997; 66: 464SB477S.
20. Sudfeld CR, Navar AM, et al. Effectiveness of measles vaccination and vitamin A treatment. Int J Epidemiol 2010 Apr; 39 Suppl 1: i48-55.
21. Barclay AJG, Foster A, et al. Vitamin A supplements and mortality related to measles: a randomised clinical trial. BMJ 1987 Jan 31; 294: 294-96.
22. Newhouse, M, et al. A case control study of carcinoma of the ovary. Brit J Prev Soc Med 1977; 31: 148-53.
23. West RO. Epidemiologic study of malignancies of the ovaries. Cancer 1966; 19: 1001-1007.
24. Classen JB, Classen DC. Clustering of cases of insulin dependent diabetes (IDDM) occurring three years after hemophilus influenza B (HiB) immunization support causal relationship between immunization and IDDM. Autoimmunity July 2002; 35(4): 247-53.
25. Classen JB, Classen DC. Clustering of cases of type 1 diabetes mellitus occurring 2-4 years after vaccination is consistent with clustering after infections and progression to type 1 diabetes mellitus in autoantibody positive individuals. J Pediatr Endocrinol Metab 2003 Apr-May; 16(4): 495-508.
26. Shaw CA, Tomljenovic L. Aluminum in the central nervous system (CNS): toxicity in humans and animals, vaccine adjuvants, and autoimmunity. Immunol Res 2013 Jul; 56(2-3): 304-16.
27. Tomljenovic L, Shaw CA. Do aluminum vaccine adjuvants contribute to the rising prevalence of autism? J Inorg Biochem 2011 Nov; 105(11): 1489-99.
28. Gherardi RK, Authier F. Macrophagic myofasciitis: characterization and pathophysiology. Lupus 2012 Feb; 21(2): 184-89.
29. Petrik MS, Wong MC, et al. Aluminum adjuvant linked to Gulf War illness induces motor neuron death in mice. Neuromolecular Med 2007; 9(1): 83-100.
30. CDC. National Vital Statistics Reports 2013 May 8; 61(4): Table 10.
31. Miller NZ. Vaccine Safety Manual for Concerned Families and Health Practitioners. (New Atlantean Press, 2015): 114-118; 143-154.


Comment: Read more information on the topic, Measles: A rash of misinformation: