
Soldiers serving with coalition forces in Afghanistan and Iraq know only too well how devastating bombs can be. The effect of shrapnel on bodies - amputated limbs, broken bones, lacerated and burned flesh - is plain enough. Less obvious and harder to understand are the long-term effects of the shock wave on the brain.
Weeks, months, or sometimes years after being concussed in an explosion, thousands of soldiers are reporting a mysterious clutch of problems. Dubbed post-concussion syndrome (PCS), symptoms include memory loss, dizziness, headaches, unexplained pains, nausea, disturbance of sleep, inability to concentrate and emotional problems.
The US military and veterans' groups see PCS as a growing problem, and the US government is pouring millions of dollars into investigating it. Some doctors, however, particularly in the UK, believe that for many patients the symptoms ascribed to PCS are not caused by concussion at all, but by the shock and stress of wartime events. It may even be getting mixed up with post-traumatic stress disorder (PTSD), an acknowledged psychological reaction to disturbing events. "Some people are saying it's a hideous mistake and that we're talking up a problem," says Simon Wessely, a psychiatrist and director of the King's Centre for Military Health Research at King's College London.
Battlefield explosions are nothing new either. For soldiers serving in Iraq and Afghanistan, one of the biggest threats they face is from roadside bombs, often improvised from cast-off artillery shells or other weapons. While more soldiers than ever are surviving such blasts, thanks to better body and vehicle armour, they are often left with concussion, or mild traumatic brain injury (mTBI) as it is usually termed in this context.
In the 1990s, soldiers returning from the first Gulf war started to report persistent cognitive problems after an mTBI. The Brain Injury Association of America and others have described mTBI as a "signature injury" of the Iraq and Afghanistan conflicts. Veterans organisations have voiced growing concerns and are even using words like "epidemic".
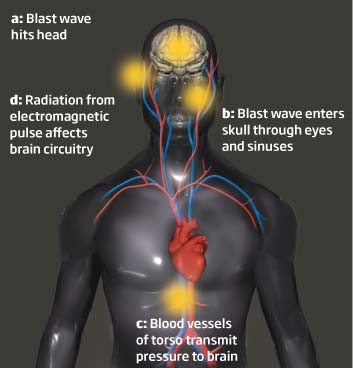
But why should a bomb blast be more likely to trigger PCS than a sports injury? The jury is still out, although various theories are being investigated (See Blasted). Despite the uncertainties, the US military, government and patient groups designate mTBI and PCS as battlefield disabilities with a high priority. The Defense and Veterans Brain Injury Center (DVBIC) in Washington DC was set up in 1992 to help military personnel with brain injuries. In 2007, the US Congress agreed to provide $900 million for research into and treatment of battlefield traumatic brain injuries and PTSD. Then in 2008, President George W. Bush reauthorised the Traumatic Brain Injury Act, which compels federal health bodies to improve care and treatment of both civilians and soldiers suffering brain injuries and to fund monitoring and research.
Meanwhile, attempts to identify soldiers with mTBI have been stepped up. Both the British and the American military routinely carry out simple mental tests on soldiers exposed to blasts, investigating symptoms and what they remember of the event. Anyone with concussion should be removed from combat and given light duties until they recover. "The key is to limit the exposures [to concussion] and limit the exposures that come on top of each other," says Jeffrey Barth, a neuropsychologist at the University of Virginia, Charlottesville, and an expert on concussion injuries.
The US army also screens for symptoms of mTBI when soldiers return from a tour of duty, and again three months later. The army is also carrying out neurocognitive tests on recruits before they are sent into combat so that doctors can check for deterioration in later tests. However, even if PCS is diagnosed there is no specific treatment. All doctors can do is target individual symptoms, for example, with antidepressants, analgesics and sleeping pills, as well as psychotherapy and behavioural therapy. And the intense focus on identifying cases of mTBI and PCS belies the fact that the mechanism by which mTBI could lead to PCS is still unclear. PCS is not so much a discrete entity as a constellation of symptoms that overlap widely with other mental and physical illnesses. There is no blood test or brain scan that can diagnose it - doctors can only ask if the patient ever had an mTBI, run through the check-list of symptoms, and rule out other causes.
Those sceptical about PCS do not dispute that a worryingly large number of soldiers are returning from Iraq and Afghanistan with persistent cognitive problems. What they question is whether these symptoms can be attributed to an mTBI. "There was this sudden view that we'd stumbled on something completely new," says Wessely. "But blasts are not a new problem in warfare."
The debate has heated up in the past year with the publication of three studies that have cast doubt on the view that PCS is a direct consequence of concussion. In one, a team at Macquarie University looked at 175 civilians admitted to hospital because of physical injuries (Journal of Neurology, Neurosurgery and Psychiatry, vol 79, p 300). About half of the group had sustained an mTBI, and after a few days 43 per cent of them had symptoms consistent with PCS. But 44 per cent of the other group, whose injury was not brain related, also had these symptoms. While this study looked at patients in the first few days after their trauma rather than months, it shows that PCS symptoms aren't necessarily the result of brain injuries.
The other two papers are perhaps more significant as they involve large epidemiological studies in soldiers, rather than civilians, and looked at symptoms over the long term. Both research teams concluded that persistent cognitive problems after an mTBI were in most cases due to psychological causes such as depression and PTSD.
In the first study, researchers questioned more than 2500 US infantry soldiers three to four months after they returned from a year-long tour of duty in Iraq, asking them about their combat experience, any injuries they had suffered and any persistent symptoms. Around 15 per cent of them had suffered an mTBI, and these soldiers had significantly more mental and physical problems than those with other injuries (The New England Journal of Medicine, vol 358, p 453). Charles Hoge at the Walter Reed Army Institute of Research in Silver Spring, Maryland, who led the study, thinks the primary cause of their ill health was probably not concussion but "exposure to a very intense traumatic event that significantly increases the risk of PTSD".
Hoge reasons that PTSD is a more likely cause than mTBI, having many common symptoms. In addition, the psychological symptoms of PTSD persist, while the effects of concussion usually disappear quickly. "When a soldier gets concussed as a result of a blast on the battlefield, that is clearly a close call," says Hoge. "Such traumatic events can set up a cascade of neurochemical events that happen with PTSD, and that can lead to a host of symptoms."
I saw dead people
The second study, by Wessely's team, which looked at nearly 6000 British soldiers who had served in Iraq in 2003, reached similar conclusions (Psychological Medicine, DOI: link). The researchers found no indication that the symptoms ascribed to PCS were caused by an mTBI. While many of those who reported such symptoms had indeed been caught in a blast, some had not. In fact, blast exposure proved no more predictive of PCS symptoms than other stressful combat situations, such as seeing dead bodies or knowingly being exposed to depleted uranium. The findings suggest that the symptoms "are most often an expression of psychological distress", says Wessely.
Michael Jaffee, however, who is national director of the DVBIC, warns against assuming that the symptoms ascribed to PCS are caused exclusively by either an mTBI or by PTSD. Since any kind of combat injury raises the risk of PTSD, and since you are more likely to show PTSD symptoms after a head injury, "there is bound to be overlap", he says.
Jaffee wonders if there might be something about blast-induced brain injury that makes people more vulnerable to psychological disorders, and to PTSD in particular. PTSD is characterised by impaired function in parts of the prefrontal cortex that help regulate how we deal with fear and anxiety and mTBI often involves damage to the prefrontal cortex. Jaffee and others suggest that this sort of damage may disrupt a person's capacity to deal with fear and thus make them more susceptible to PTSD (Journal of Rehabilitation Research and Development, vol 44, p 895).
Wessely questions this kind of association because "when you get concussion you lose your memory, so how can you have flashbacks when you don't remember the incident?". But concussion does not always involve amnesia. Furthermore, Hoge says, traumatic memories can trigger PTSD even when you are not conscious of them.
In any case, does it matter to the patient what the cause of their symptoms is? Many researchers say it matters a great deal. Plenty of studies have shown that what you tell a patient about what is wrong with them has a big influence on how long they take to get better. "If they believe they are going to have lifelong impairment as a result of a brain injury, they are more likely to have persistent symptoms," says Hoge. "On the other hand, individuals who have positive expectations, who are told they are going to get better, actually do better."
Wessely and Hoge even avoid the term mTBI when talking to patients. "The phrase 'traumatic brain injury' makes it sound like you have shrapnel in your skull and will end up in a wheelchair," says Wessely. "Call it concussion and they'll think, I had that playing rugby."
Another reason why understanding the true cause of PCS matters relates to whether it should be screened for. The US military screening programmes have found that up to 18 per cent of its returning personnel have had an mTBI. Figures from the UK military, on the other hand, which does not carry out mass screening, suggest that fewer than 1 per cent of its troops have suffered an mTBI.
Why such a big difference? It is possible, of course, that US troops get blown up more, or perhaps have weaker protective helmets. But another explanation is that US doctors find more head injuries simply because they have systematic screening in place, while British soldiers have to decide they have a problem and take the action of going to see their doctor.
So might the US be overdiagnosing the problem, or the UK underdiagnosing it? Lionel Jarvis, the UK's assistant chief of the UK defence staff (health), thinks the former. Jarvis points out that any soldier returning from a six-month tour of duty in Afghanistan, where they've been away from their family and in an extreme, high-pressure environment, is likely to show symptoms of distress: "How on earth do you unpick the different symptoms and explain whether they are due to a head injury or one of a large number of other potential causes?"
Wessely says his study showed that screening soldiers for PCS when they get home cannot distinguish between those whose problems were caused by concussion and those who have anxiety, depression or PTSD. "It's fraught with danger," he says. "Caution is needed before labelling mTBI as an epidemic because this might become self-fulfilling."
But Barth insists some kind of screening is needed. "At least the military is making an attempt to look at these issues," he says.
When it comes to combat trauma, unpicking the physical from the psychological is bound to be highly complex. As Barth says, perhaps the greatest danger could be in trying to simplify the picture too much. "I recommend that we get comfortable with the complexity," he says, "and treat it as a challenge."


Reader Comments
to our Newsletter